
A cephalometric study to evaluate and compare the effect of upper premolar extraction on pharyngeal airway dimension in skeletal class I and class II patients
Rahul Paul 1![]()
![]() ,
Deepti Yadav 2
,
Deepti Yadav 2![]()
![]() ,
Priya Kishore 3
,
Priya Kishore 3![]() , Ish Kumar Sharma 4
, Ish Kumar Sharma 4![]()
![]() ,
Vandana Gulia 4
,
Vandana Gulia 4![]()
![]() ,
Prakher Saini 5
,
Prakher Saini 5![]()
![]()
1 Professor
and Head of the Department, Department of Orthodontics and Dentofacial Orthopaedics, Inderprastha Dental
College and Hospital, Ghaziabad, Uttar Pradesh, India
2 Professor,
Department of Orthodontics and Dentofacial Orthopaedics,
Inderprastha Dental College and Hospital, Ghaziabad,
Uttar Pradesh, India
3 Post graduate student, Department of Orthodontics and Dentofacial Orthopaedics, Inderprastha Dental College and Hospital, Ghaziabad, Uttar Pradesh, India
4 Reader, Department of Orthodontics and Dentofacial Orthopaedics, Inderprastha Dental College and Hospital, Ghaziabad, Uttar Pradesh, India
5 Senior Lecturer, Department of Orthodontics and Dentofacial Orthopaedics, Inderprastha Dental College and Hospital, Ghaziabad, Uttar Pradesh, India
|
|
ABSTRACT |
||
|
The goal of
this study was to evaluate and compare the effect of upper premolar
extraction on pharyngeal airway dimension in skeletal class I and class II
malocclusion patients. This retrospective study analyzed pre- and
post-treatment orthodontic records of patients with skeletal Class I and
Class II malocclusions to assess changes in the pharyngeal airway. ANB and
WITS appraisal was employed to determine the skeletal pattern. Measurement
parameters of Pharyngeal airway dimensions like superior, middle and inferior
airway space were evaluated and compared between the two malocclusions. Lateral cephalograms of 100 patients (50
with Class I and 50 with Class II malocclusion) aged 18–26 years were used to
measure airway dimensions, and data was compared to evaluate the impact of
orthodontic treatment on pharyngeal space. Pre- and post-treatment
cephalograms were obtained using standardized exposure settings and patient
positioning. The data was analyzed using software SPSS 27.0 with
Non-parametric test and the Wilcoxon signed-rank test at a 5% significance
level was used. The results indicated that pharyngeal airway dimensions in
skeletal Class I patients had a wider airway than Class II patients. Also,
before treatment, Class I malocclusion patients had a wider pharyngeal airway
than Class II patients while After-treatment, both groups experienced airway
reduction, with Class I patients showing a more significant decrease. |
|||
|
Received 05 March 2025 Accepted 10 April
2025 Published 31 May 2025 Corresponding Author Deepti
Yadav, deepti.yadav@yahoo.com DOI 10.29121/granthaalayah.v13.i5.2025.6169 Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2025 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
Keywords: Retrospective Studies, Pharynx, Bicuspid,
Malocclusion |
|||
1. INTRODUCTION
Modern orthodontics has extensively explored the relationship between skeletal malocclusions, encompassing Class I, II, and III, and also took into account the morphology of their soft tissues. Paul et al. (2025) The pharyngeal airway refers to the anatomical passage through which air travels from the nose and mouth to the lungs. It includes three primary segments: the nasopharynx, oropharynx, and laryngopharynx, each with distinct functional roles in respiration and speech. Berkovitz and Moxham (1988) The patency, or openness, of the pharyngeal airway is critical for adequate oxygen exchange and the prevention of airway obstructions, which may contribute to various conditions, including obstructive sleep apnea (OSA). Sankri (2012)The development of the pharyngeal airway occurs in tandem with overall craniofacial growth. During the early stages of life, facial structures including the maxilla, mandible, and the surrounding soft tissues undergo dynamic growth, which affects the shape and structure of the pharyngeal passage. As the individual ages, changes in the musculoskeletal framework and soft tissue structures can alter the size and shape of the airway. Chuang et al. (2022) Solow’s hypothesis suggests that changes in the head posture, jaw, or tongue can affect the soft tissues in the oral and pharyngeal regions. This shift in posture alters the breathing pattern, causing the tongue and lower jaw to move downward while the head extends forward. Sana et al. (2022) Skeletal discrepancies, such as maxillary retrusion or mandibular deficiencies, may lead to reduced pharyngeal airway dimensions, potentially predisposing individuals to breathing disorders like OSA. Rodrigues et al. (2024) Individuals having Skeletal Class I malocclusion generally have more favorable airway dimensions, reflecting their balanced skeletal structure. In contrast patients having Skeletal Class II malocclusion typically display reduced airway volume and smaller cross-sectional areas, especially in the nasopharyngeal and oropharyngeal regions. The retruded mandible often seen in Class II cases can cause the tongue to shift posteriorly, further narrowing the space. As the nasopharynx becomes deeper, its back wall becomes more constricted. Moreover, people with Class I and Class II malocclusions or hyper divergent maturation typically have much constricted upper pharyngeal passage than those with natural development. de Freitas et al. (2006)The primary reasons for seeking orthodontic treatment are functional efficiency, aesthetic harmony, and structural balance. Yadav et al. (2024) Additionally, orthodontic interventions aimed at modifying craniofacial structures are known to have direct effects on airway morphology. Shen et al. (2023) When the upper airway becomes narrower, it can increase airflow resistance, potentially raising the susceptibility to snoring and, in more extreme scenarios can cause obstructive sleep apnea.
As an orthodontic intervention premolar extraction is a common orthodontic procedure performed to alleviate dental crowding and correct protrusive profiles. Treatments that involve anterior teeth retraction, such as in cases of premolar extraction, may cause result in a decrease in the pharyngeal passage size, especially in those having any pre-existing airway limitations. Bhatia et al. (2016) For instance, mandibular advancement procedures, which are often employed to treat Class II malocclusion, may result in an expansion in airway volume and improve airway patency. Qahtani (2016) Therefore, orthodontic treatment, particularly interventions aimed at altering maxillomandibular relationships, has a direct impact on the pharyngeal airway. Shift in tooth alignment and jaw structure can affect both the dimensions and form of the airway. Such changes are likely to influence the position of the tongue, which in turn may affect the pharyngeal passage space. Despite the recognized potential for these changes to occur, there is a lack of comprehensive research on the specific effects that anterior teeth retrusion and the resulting dentofacial changes have on the pharyngeal airway dimensions. By initiating early orthodontic treatment, we can positively influence jaw growth and tongue posture, which helps in modifying and improving pharyngeal airway dimensions. This proactive approach can reduce the risk of airway-related issues such as mouth breathing, snoring, and even obstructive sleep apnea later in life. Early intervention allows for proper alignment and development of the dental arches, supporting better airway function and overall health.
2. POST OCCUPANCY EVALUATION (POE)
This retrospective study was conducted by analyzing the pre-treatment and post-treatment records of skeletal Class I and Class II patients (based on ANB and WITS analysis), aged 18–26 years, who had undergone orthodontic treatment involving first premolar extraction. Cephalometric parameters were analyzed at T0 (pre-treatment) and T1 (post-treatment) Figure 1 The lateral cephalograms were taken with the CS 8000C system with standardized exposure settings (90 kV, 15 mA, 0.500 seconds) and consistent head positioning for accuracy. A single examiner recorded the readings. Observer reliability was ensured by initially tracing a random sample of 10 cephalograms before completing the full analysis.
Parameters which were used for classifying Class I and class II into group A and group B was defined by ANB and WITS appraisal. ANB angle is the angle formed by Nasion, point A and point B if the angle ranges 2º± 2, then it is considered as skeletal class I while Class II have an ANB angle greater than 4 degrees. Wits Appraisal is the distance between points A and point B measured on the occlusal plane. According to this measurement, values of -1mm for men and 0mm for women is considered as skeletal class I and values > -1mm for men and values > 0mm for women are considered as skeletal class II.
Pharyngeal airway dimensions were manually traced and measured from lateral cephalograms. For purpose of the study and correlation with skeletal parameters pharyngeal airway analysis was done and following parameters were evaluated. Figure 2
1) Tongue length (TGL): A line drawn from the tip of the tongue (TT) to the deepest point at the base of the epiglottic fold (EpB).
2) Tongue height (TGH): A perpendicular line from the dorsum of the tongue to the TGL, representing the maximum thickness of the tongue.
3) Soft palate length (SPL): Line extending from posterior nasal spine to tip of uvula (P)
4) Soft palate thickness (SPT): Maximum thickness of soft palate along a line perpendicular to posterior nasal spine (PNS) and tip of uvula
5) Superior posterior airway space (SPAS): A line drawn from the mid-point of dorsum of the soft palate to the posterior wall of the pharynx.
6) Middle airway space (MAS): A line passing through tip of uvula to posterior pharyngeal wall
7) Inferior airway space (IAS): A line extending through the posterior pharyngeal wall and the point where the posterior contour of the tongue meets the mandibular angle.
8) Vertical airway length (VAL): The distance between PNS and deepest point in the base of the epiglottic fold.
Figure 1
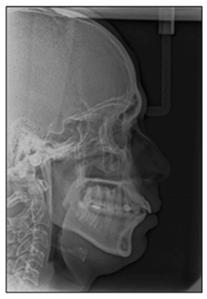
|
Figure 1 Lateral Cephalogram |
Figure 2
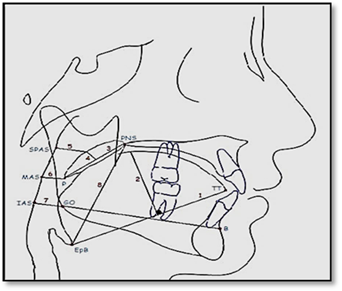
|
Figure 2 Pharyngeal Airway Space |
The metrics for this research was recorded in Microsoft Excel 2010 and analysis was done with SPSS statistical software version 27.0. Descriptive statistics comprised calculations of frequency and percentage. Kolmogorov Smirnov test was used to check the normality of the data. Since the values did not follow a normal distribution, a non-parametric test was employed for analysis. The Wilcoxon signed-rank test was applied to evaluate the pre-treatment and post-treatment data obtained during the course. The significance level for this research was set at 5%.
3. FINDINGS AND DISCUSSION
The study analyzed pharyngeal passage parameters to evaluate how orthodontic intervention involving premolar extraction influences the upper respiratory tract in Skeletal Class I and Skeletal Class II patterns. The evaluation focused on key parameters, including the Superior Posterior Airway Space (SPAS), Middle Airway Space (MAS), Inferior Airway Space (IAS), and Vertical Airway Length (VAL), to determine whether the treatment led to significant changes in airway dimensions.
On intragroup comparison of pharyngeal airway space parameter in class I before and after premolar extraction, SPAS (-2.38 ± 1.259, p < 0.001 ); VAL ( 4.12 ± 1.272, p < 0.001); TGL (-1.34 ± 0.871, p < 0.001 ); TGH (0.9 ± 1.073, p < 0.001); SPL (-1.02 ± 0.684, p < 0.001); SPT (-0.84 ± 0.865, p < 0.001) showed significant difference whereas no significant difference was observed in MAS (-0.08 ± 0.944, p=0. .312) and IAS (0.36 ± 3.205, p=0.508). similarly on comparing pharyngeal airway space parameter in class II before and after premolar extraction, SPAS (-2.46 ± 1.215, p < 0.001); MAS (-2.22 ± 1.130, p < 0.001 ); VAL (3.14 ± 0.969, p < 0.001); TGL (-1.12 ± 0.961, p < 0.001); TGH (1 ± 0.765, p < 0.001); SPL (-0.96 ± 0.807, p < 0.001); SPT (-1.02 ± 0.714, p < 0.001) showed significant difference . On the contrary, IAS showed no significant difference (0.92 ± 3.318, p= 0.058) Table 1, Graph 1,Graph 2
Table 1
|
Table 1 Changes in Pharyngeal Airway Dimension in Group A and Group B Before and After Orthodontic Treatment |
||||||
|
Variables |
Group |
Pre-Treatment Mean ±
SD |
Post-Treatment Mean ±
SD |
Mean Difference ± SD |
p-value |
S/NS |
|
A |
20.640 ± 3.2056 |
18.260 ± 3.0426 |
-2.38 ± 1.259 |
<0.001 |
HS |
|
|
SPAS |
B |
13.780 ± 1.4327 |
11.320 ± 1.8892 |
-2.46 ± 1.215 |
<0.001 |
HS |
|
A |
13.940 ± 1.9210 |
13.860 ± 1.9379 |
-0.08 ± 0.944 |
0.312 |
NS |
|
|
MAS |
B |
10.840 ± 1.8111 |
8.620 ± 1.8940 |
-2.22 ± 1.130 |
<0.001 |
HS |
|
A |
12.480 ± 3.0987 |
12.840 ± 3.0663 |
0.36 ± 3.205 |
0.508 |
NS |
|
|
IAS |
B |
10.840 ± 1.8111 |
11.760 ± 2.8180 |
0.92 ± 3.318 |
0.058 |
NS |
|
A |
59.200 ± 3.1493 |
63.320 ± 3.5768 |
4.12 ± 1.272 |
<0.001 |
HS |
|
|
VAL |
B |
58.760 ± 4.2357 |
61.900 ± 4.2630 |
3.14 ± 0.969 |
<0.001 |
HS |
|
A |
68.960 ± 5.2449 |
67.620 ± 4.9729 |
-1.34 ± 0.871 |
<0.001 |
HS |
|
|
TGL |
B |
65.080 ± 6.3498 |
63.960 ± 6.3018 |
-1.12 ± 0.961 |
<0.001 |
HS |
|
A |
27.200 ± 2.9623 |
28.360 ± 3.0086 |
0.9 ± 1.073 |
<0.001 |
HS |
|
|
TGH |
B |
32.240 ± 3.2423 |
31.340 ± 3.5145 |
1 ± 0.765 |
<0.001 |
HS |
|
A |
27.120 ± 3.1985 |
26.100 ± 3.3700 |
-1.02 ± 0.684 |
<0.001 |
HS |
|
|
SPL |
B |
25.600 ± 2.5071 |
24.640 ± 2.5932 |
-0.96 ± 0.807 |
<0.001 |
HS |
|
A |
6.000 ± 1.3401 |
5.160 ± 1.4758 |
-0.84 ± 0.865 |
<0.001 |
HS |
|
|
SPT |
B |
4.920 ± 1.3529 |
3.900 ± 1.2657 |
-1.02 ± 0.714 |
<0.001 |
HS |
Graph 1
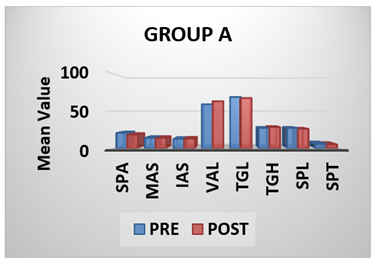
|
Graph 1 Changes in Pharyngeal Airway Dimension in Group A |
Graph 2
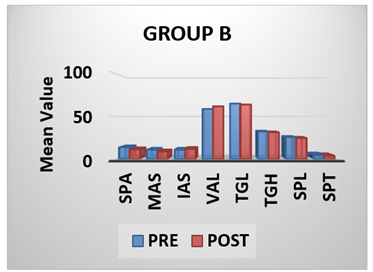
|
Graph 2 Changes in Pharyngeal Airway Dimension in Group B |
Table 2
|
Table 2 Comparison Between the Pharyngeal Airway Dimension in Skeletal Class I and Class II Malocclusion Patients Before and After Orthodontic Treatment Following Extraction of Upper First Premolar |
||||
|
VARIABLES |
Pre (Mean +SD) |
Post (Mean +SD) |
Mean Difference
pre-post (Mean +SD) |
|
|
SPAS |
GROUP A |
20.6+3.205 |
18.2+3.042 |
2.38+1.260 |
|
GROUP B |
13.7+1.432 |
11.3+1.889 |
2.46+1.216 |
|
|
MAS |
GROUP A |
13.9+1.921 |
13.8+1.937 |
0.08+0.944 |
|
GROUP B |
10.8+1.811 |
8.62+1.894 |
2.22+1.130 |
|
|
IAS |
GROUP A |
12.4+3.098 |
12.8+3.066 |
2.846 |
|
GROUP B |
10.8+1.811 |
11.7+2.818 |
2.399 |
|
|
VAL |
GROUP A |
59.2+3.149 |
63.3+3.576 |
-2.848 |
|
GROUP B |
58.7+4.235 |
61.9+4.263 |
-2.171 |
|
|
TGL |
GROUP A |
68.9+5.244 |
67.6+4.972 |
1.34+0.872 |
|
GROUP B |
65+6.349 |
63.9+6.301 |
1.12+0.961 |
|
|
TGH |
GROUP A |
31.3+3.514 |
32.2+3.242 |
-0.394 |
|
GROUP B |
27.2+2.962 |
28.3+3.008 |
0.90+1.074 |
|
|
SPL |
GROUP A |
27.1+3.198 |
26.1+3.370 |
1.02+0.685 |
|
GROUP B |
25.6+2.507 |
24.6+2.593 |
0.96+0.807 |
|
|
SPT |
GROUP A |
6+1.340 |
5.16+1.475 |
0.84+0.866 |
|
GROUP B |
4.92+1.352 |
3.9+1.265 |
1.02 +0.714 |
|
|
p ≤ 0.05 – Significant, CI = 95 % |
||||
On intergroup comparison between Class I and Class II patients, the mean difference in SPAS (2.42 ± 1.232, p = 0.883) showed no significant difference, indicating that the reduction in superior pharyngeal airway space post-treatment was similar between both skeletal patterns. Similarly, no statistically significant difference was observed in IAS (0.64 ± 3.258, p = 0.208), TGL (1.23 ± 0.920, p = 0.342), SPL (0.99 ± 0.745, p = 0.825), and SPT (0.93 ± 0.795, p = 0.226), suggesting comparable changes in inferior airway space, tongue length, and soft palate morphology between the groups.
However, statistically highly significant intergroup
differences were observed in MAS (1.15 ± 1.493, p < 0.001), VAL
(-3.63 ± 1.228, p < 0.001), and TGH (-0.13 ± 1.390, p < 0.001),
indicating that Class II patients experienced significantly greater reductions
in middle airway space and different patterns of change in vertical airway
length and tongue height compared to Class I patients
Table 2, Graph 3.
Graph 3
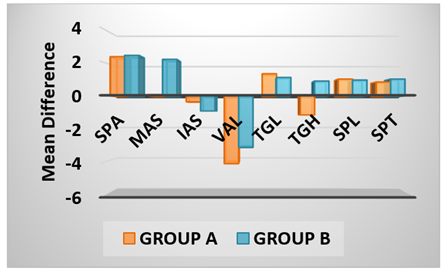
|
Graph 3 Comparison Between the Pharyngeal Airway Dimension in Skeletal
Class I and Class II Malocclusion Patients Before and After Orthodontic
Treatment Following Extraction of Upper First Premolar |
The primary reasons for seeking orthodontic treatment are functional efficiency, aesthetic harmony, and structural balance. Yadav et al. (2024) Several factors can impact the positioning of the tongue and soft palate, which in turn may influence the size of the airway. Aspects such as breathing habits, body weight, age, sex, tongue enlargement, and genetic predisposition can either widen or narrow the airway. Paul et al. (2015) One of the main considerations is that modifying the anterior tooth alignment and oral musculature through extraction may also alter tongue placement, which could ultimately affect airway size. A study by Patel P et al. Patel et al. (2017) suggested that retracting the anterior teeth backward reduces arch length, causing the anterior boundary of the oral cavity to shift towards the throat. To minimize the influence of growth, the study focused on individuals aged 16 to 25 years, an age range where pharyngeal morphology is typically fully developed. This age selection aimed to provide a more accurate assessment of how extractions affect airway size. The lateral cephalograms were classified into Class I and Class II skeletal patterns based on the ANB angle, as this measurement is widely recognized and frequently utilized to assess the anteroposterior association among maxilla and mandible. Kim et al. (2010),El and Palomo (2011)
Research on individuals with skeletal Class I malocclusion found that orthodontic treatment led to a statistically significant decrease in the superior posterior pharyngeal space (SPAS). This reduction in airway size may be linked to the backward movement of the tongue resulting from the retraction of front teeth. This tongue movement could exert pressure on the soft palate, causing changes in the airway. These results suggest that orthodontic treatment involving tooth retraction can decrease intraoral space, consequently reducing pharyngeal volume. Similar reductions in SPAS following orthodontic treatment were reported in studies by Nasser A et al. Nasser et al. (2019) and Patel P et al. Patel et al. (2017) However, Aldosari MA et al. Aldosari et al. (2020) observed a slight, non-significant increase in SPAS after treatment.
In individuals with skeletal Class I malocclusion, research indicated a significant increase in vertical airway length (VAL) following different orthodontic management approaches. Aldosari MA et al. Aldosari et al. (2020) also reported a similar increase in VAL. However, these findings contrast with those of AlMaaitah et al. Al Maaitah et al. (2012), who found no significant changes in airway dimensions, including vertical airway length, after orthodontic treatment. A significant reduction was observed in TGL, SPL, and SPT, while TGH showed a notable increase in skeletal Class I malocclusion following treatment. Similar results were reported by Nasser A et al. Nasser et al. (2019), who noted a significant rise in TGH along with a significant decline in TGL, SPL, and SPT.
4. OBSERVATIONS
· In patients with skeletal Class I malocclusion, the pharyngeal airway was larger before treatment than after undergoing orthodontic intervention that involved removal of the upper first premolars.
· In patients with skeletal Class II malocclusion, the pharyngeal airway dimension was larger before treatment than after undergoing orthodontic intervention that involved removal of the upper first premolars.
· Before orthodontic treatment, patients with skeletal Class I malocclusion had a larger pharyngeal airway dimension compared to those with skeletal Class II malocclusion.
· The pharyngeal airway dimension was found to be greater in skeletal class I malocclusion patients as compared to the skeletal class II malocclusion patients after orthodontic intervention that involved removal of upper first premolars.
CONFLICT OF INTERESTS
None.
ACKNOWLEDGMENTS
None.
REFERENCES
Al Maaitah, E., El Said, N., & Abu Alhaija, E. S. (2012). First Premolar Extraction Effects on Upper Airway Dimension in Bimaxillary Proclination Patients. The Angle Orthodontist, 82(5), 853-859. https://doi.org/10.2319/101711-646.1
Aldosari, M. A., Alqasir, A. M., Alqahtani, N. D., Almosa, N. A., Almoammar, K. A., & Albarakati, S. F. (2020). Evaluation of the Airway Space Changes after Extraction of four Second Premolars and Orthodontic Space Closure in Adult Female Patients with Bimaxillary Protrusion: A Retrospective Study. Saudi Dental Journal, 32(3), 142-147. https://doi.org/10.1016/j.sdentj.2019.11.004
Almurtadha, R. H., Alhammadi, M. S., Fayed, M. M. S., Abou-El-Ezz, A., & Halboub, E. (2018). Changes in soft Tissue Profile After Orthodontic Treatment with and Without Extraction: A Systematic Review and Meta-Analysis. Journal of Evidence-Based Dental Practice, 18(3), 193-202. https://doi.org/10.1016/j.jebdp.2017.09.002
Berkovitz, B. K., & Moxham, B. J. (1988). The Mouth, Palate, and Pharynx. In A Textbook of Head and Neck Anatomy 272-331.
Bhatia, S., Jayan, B., & Chopra, S. S. (2016). Effect of Retraction of Anterior Teeth on Pharyngeal Airway and Hyoid Bone Position in Class I Bimaxillary Dentoalveolar Protrusion. Medical Journal Armed Forces India, 72, S17-S23. https://doi.org/10.1016/j.mjafi.2016.06.006
Chuang, Y. J., Hwang, S. J., Buhr, K. A., Miller, C. A., Avey, G. D., Story, B. H., et al. (2022). Anatomic Development of the Upper Airway During the First Five Years of life: A Three-Dimensional Imaging Study. PLoS ONE, 17(3), e0264981. https://doi.org/10.1371/journal.pone.0264981
El, H., & Palomo, J. M. (2011). Airway Volume for Different Dentofacial Skeletal Patterns. American Journal of Orthodontics and Dentofacial Orthopedics, 139(6), e511-e521. https://doi.org/10.1016/j.ajodo.2011.02.015
Flores-Blancas, A. P., Carruitero, M. J., & Flores-Mir, C. (2017). Comparison of Airway Dimensions in Skeletal Class I Malocclusion Subjects with Different Vertical Facial Patterns. Dental Press Journal of Orthodontics, 22(6), 35-42. https://doi.org/10.1590/2177-6709.22.6.035-042.oar
Kim, Y. J., Hong, J. S., Hwang, Y. I., & Park, Y. H. (2010). Three-Dimensional Analysis of Pharyngeal Airway in Preadolescent Children with Different Anteroposterior Skeletal Patterns. American Journal of Orthodontics and Dentofacial Orthopedics, 137(3), 306.e1. https://doi.org/10.1016/j.ajodo.2009.10.026
Nasser, A., Alshammari, R., Al-Jewair, T., Aldosari, M., & Sahar, A. (2019). Post-Orthodontic Pharyngeal Airway Changes Following First Premolar Extraction and Incisor Retraction in Bimaxillary Protrusion Patients: A Retrospective Study. Journal of Research in Medical and Dental Science, 7(5), 29-38.
Patel, P., Nagarag, K., Jain, A., Doshi, D., & Ringane, A. (2017). Assessment of Cephalometric Changes in Pharyngeal Airway Involving First Premolar Extractions in Class II Division 1 Patients and Class I Bimaxillary Protrusion Patients Treated with Fixed Mechanotherapy: A Retrospective Study. Indian Journal of Orthodontics and Dentofacial Research, 3(1), 31-33. https://doi.org/10.18231/2455-6785.2017.0006
Paul, D., Varma, S., & Ajith, V. V. (2015). Airway in Class I and Class II Skeletal Pattern: A Computed Tomography Study. Contemporary Clinical Dentistry, 6(3), 293-298. https://doi.org/10.4103/0976-237X.161856
Paul, R., Yadav, D., Gupta, M., Sharma, I. K., Gulia, V., Kishore, P., & Chhabra, A. (2025). Evaluation of Lip Print Patterns, Lip Strain, and Lip Thickness in Skeletal Class I and class II Malocclusion. Cuestiones de Fisioterapia, 54(4), 5947-5958.
Qahtani, N. D. A. (2016). Impact of Different Orthodontic Treatment Modalities on Airway: A Literature Review. Pakistan Journal of Medical Sciences, 32(1), 249-252. https://doi.org/10.12669/pjms.321.8743
Rodrigues, J., Evangelopoulos, E., Anagnostopoulos, I., Sachdev, N., Ismail, A., Samsudin, R., et al. (2024). Impact of class II and class III Skeletal Malocclusion on Pharyngeal Airway Dimensions: A Systematic Literature Review and meta-analysis. Heliyon, 10(6), e27284. https://doi.org/10.1016/j.heliyon.2024.e27284
Ruellas, A. C. D. O., Ruellas, R. M. D. O., Romano, F. L., Pithon, M. M., & Santos, R. L. D. (2010). Extrações Dentárias em Ortodontia: Avaliação de Elementos de Diagnóstico. Dental Press Journal of Orthodontics, 15(3), 134-157. https://doi.org/10.1590/S2176-94512010000300017
Sana, S., Kondody, R. T., Swamy, K., & Fatima, A. (2022). Evaluation and Correlation Between Pharyngeal Space, Mandible, and Tongue in two Different Facial Patterns. Journal of Indian Orthodontic Society, 56(4), 351-358. https://doi.org/10.1177/03015742221083065
Sankri-Tarbichi, A. G. (2012). Obstructive Sleep Apnea-Hypopnea Syndrome: Etiology and Diagnosis. Avicenna Journal of Medicine, 2(1), 3-8. https://doi.org/10.4103/2231-0770.94803
Shen, Y., Li, X., Feng, X., Yu, L., Weng, L., Zhang, C., et al. (2023). Differences in the Effects of Orthodontic Treatment on Airway-Craniocervical Functional Environment in Adult and Adolescent Patients with Skeletal Class II high-angle: A retrospective pilot study. BMC Oral Health, 23(1), 605. https://doi.org/10.1186/s12903-023-03328-w
Yadav, D., Paul, R., Sharma, I. K., & Saini, P. (2024). Correlation of type of Malocclusions and Cephalometric Parameters with Smile Characteristics in Lateral and Oblique Views. Iranian Journal of Orthodontics, 19(2), 1-10.
de Freitas, M. R., Alcazar, N. M. P. V., Janson, G., de Freitas, K. M. S., & Henriques, J. F. C. (2006). Upper and Lower Pharyngeal Airways in Subjects with Class I and Class II Malocclusions and Different Growth Patterns. American Journal of Orthodontics and Dentofacial Orthopedics, 130(6), 742-745. https://doi.org/10.1016/j.ajodo.2005.01.033
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© Granthaalayah 2014-2025. All Rights Reserved.