
PERCEIVED STIGMA, BEHAVIOURAL PROBLEM AND DEPRESSION AMONG INDIVIDUALS WITH SUBSTANCE ABUSE ATTENDING SELECTED DE-ADDICTION CENTRES, KOLKATA, WEST BENGAL
Bandana Mondal 1![]()
![]() ,
Manika Mazumder 2
,
Manika Mazumder 2![]()
![]() ,
Alpana Rani Das 3
,
Alpana Rani Das 3![]()
1 Clinical
Instructor, Health & Family Welfare Department, College of Nursing, Medical
College & Hospital, Health University, Kolkata, West Bengal, India
2 Professor,
College of Nursing, Nil Ratan Sirkar Medical College and Hospital, Kolkata,
West Bengal, India
3 Senior
Faculty, College of Nursing, Medical College and Hospital, Kolkata, West
Bengal, India
|
|
ABSTRACT |
||
|
Substance abuse is a considerable public health problem throughout the world with vast implication on public health. Its real impact is on the social and family dynamics that underlie its communities. Aim: This study aims to assess Perceived stigma, behavioural problem and depression among individuals with substance abuse attending selected de-addiction centers, Kolkata, West Bengal. Methods: A Descriptive survey design was adopted and 200 individuals with substance abuse were selected using simple random sampling technique. Data were collected using semi structured demographic Proforma, standardized perceived stigma of substance abuse scale (PSAS), standardized behavioural problem scale (BPS) and Beck’s depression Inventry. Result: The findings revealed that majority 81% individual with substance abuse had moderate perceived stigma whereas 18% had high perceived stigma and 1 % had low perceived stigma and (85% ) individuals with substance abuse were mild behavioural problem and (15%) in individuals with substance abuse were moderate behavioural problem and (41.5% ) individuals had moderate depression , ( 28% ) had borderline clinical depression , (27.5%) had mild mood disturbance ,(3%) had these ups and downs were considered normal. Result showed that there was significant association between level of depression with Regularity of treatment, life style practices with monthly family income and educational status of participants. Conclusion: The current study concludes that perceived stigma, behavioural problems and depression among individuals
with substance abuse is effective to motivational prevention in the field of
psychiatry nursing. |
|||
|
Received 22 May 2024 Accepted 02 July 2024 Published 31 July 2024 Corresponding Author Bandana Mondal,
mbandana45@gmail.com DOI 10.29121/granthaalayah.v12.i7.2024.5697 Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2024 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
Keywords: Perceived Stigma, Behavioural
Problem, Depression and Substance Abuse |
|||
1. INTRODUCTION
Substance abuse
is a major public health problem throughout the world with vast implication on
public health. According to National Mental Health Survey (NMHS)
conducted in 12 states of India, the prevalence of substance use disorders is
22.4% in those above18 years (20.9% for alcohol use disorders, 4.6% for tobacco
use disorders, 0.6% for illicit substance use disorders). Substance abuse is a
chronic, relapsing condition. It includes the use of illicit substances such as
alcohol, tobacco, diversion of prescribe drugs, as well as illicit drugs. There
is a pressing need to improve short-and long-term treatment outcome.
Sidana et al. (2021) It is well recognized as a complex psychological phenomenon an
substance dependence is considered as a 'family disease. It affects the
individual as well as those around physically, emotionally and financially. It
also leads to distress and social and occupational dysfunction.
According to the
World Health Organization (WHO) substance abuse is continual or sporadic drug
use inconsistent with or unrelated to perfect clinical exercise. World Health Organization (1994)
2. BACKGROUND OF THE STUDY
This survey record additionally advocate that Alcohol
(21.4%) was the primarily substance used (apart from tobacco) succeeded by
cannabis (3.0%) and opioids (0.7%). 17 to 26% of alcohol users qualified for
ICD 10 diagnosis criteria of dependence, translating to average prevalence of
about 4%. Tobacco use prevalence was high at 55% among males, with maximum use
in the age group of 18-50 years Luoma et al. (2002).
The Drug Abuse Monitoring system, which evaluated the primary substance of abuse in patient treatment centres found that major substance use were found that alcohol (43.9%), opioids (26%) and cannabis (11.6%). So, need of the study should be motivational to prevent substance abuse which depends on the stigmatisation of the Abuser.
Perceived
stigma is fear of being discriminated towards or the worry
of enacted stigma and arises from society’s perception Luoma et al. (2020). Research on stigma is vast and focussed on stigma directed toward members of stigmatized
group defind by race and ethnicity, homosexuality, region,
and mental illness, to name a few. Outcomes of those research imply that
reviews of stigma, whether or not enacted, perceived,
or self-stigma, may have extreme effects for people. Some of the consequences
of stigma for those with behavioral health problems include difficulties
obtaining employment Fiato (2005). The alcohol abuse and other drugs results in a multiple of problems for the abuser, family members
and the wider community. Stigma in opposition to substance use could be the potential barrier
for human beings with
substance use to seek expert help. Perceived stigma is worry of being discriminated in opposition to or the fear of enacted stigma and arises
from society’s perception. Substance use-associated
stigma has additionallyaffect the medical population Kulesza et al. (2013).
The problem
of medicine abuse has
preoccupied scholars since time old. It is a psychosocial problem that affects every society and threatens the future of the youthful people.
Drug dependency has
turned numerous youthful people
into psychopaths, zombies and culprits hence the subject to exploration.
Depressive complaints are constantly setup as a comorbidity among cases with substance abuse.
Utmost of the time it is reported as under diagnosed and a
majority of cases go undressed. Numerous studies have indicated that
comorbid depressive symptoms play a major part in the prognosis of substance
use complaint and the relapse has been setup to be greater in patients who have
a comorbid depression. The present study seeks to determine the comorbidity of
depression in cases with substance abuse and their socio-demographic features.
It is important
to realize that even the families of the substance abuser needs
help. The family is often viewed as the basic source of strength, which
provides nurturance and support for its individual members as well as ensuring
stability and generational continuity for community and culture. In reality, the family is a long way greater complex. Drinking and family functioning
are related Roberts & Linney (2000), although the relationship may be unfruitful, complimentary, iterative, or incidental to other causes. There are several family
problems that are likely to ooccur with an
individual’s alcohol abuse, including intimate partner violence, conflict and
low relationship satisfaction, economic and legal vulnerability, and child
risks Great Britain (2010).
While working in Psychiatry ward, it is seen that
the substance abuse client is considered devalued and unimportant to others then he beliefs negative thoughts. Some of consequences of perceived stigma leads to behavioural problem and depression. The stigma as a barrier
to recovery from addiction. So, the investigator think
that it is important to assess perceived stigma, behavioural
problem and depression among individuals with substance abuse persons.
3. PROBLEM STATEMENT
Perceived
stigma, behavioural problem and depression among individuals with substance
abuse attending selected de-addiction centres, Kolkata, West Bengal.
4. OBJECTIVES OF THE STUDY
1)
To
assess perceived stigma among individuals with substance abuse
2)
To
assess the behavioural problem among individuals with substance abuse
3)
To
determine the level of depression among individuals with substance abuse
4)
To find
out association between perceived stigma with selected demographic variables.
5) To find out association between depression
with selected demographic variables.
5. METHODOLOGY
Quantitative approach was adopted with descriptive survey design. The study was conducted from 13.02.23 to 09.03.23. The subjects were people between 18 - 50 years of age attending de-addiction centre of Institute of psychiatry, Lumbini Park Mental Hospital, Pavlov Hospital, Kolkata, West Bengal.
Simple random sampling technique was adopted to prefer 200 samples, were met the designated inclusion and exclusion criteria. Samples were selected from prepared frame through lottery method.
Ethical
clearance was taken from Institutional Ethical Committee of Medical College and
Hospital, Kolkata, permission for data collection were taken from MSVP of Pavlov and Lumbini Park Mental Hospital,
Kolkata and Permission also was taken from Director of Institute of Psychiatry,
Kolkata, West Bengal. Informed
consent was taken from all participants in their language. Confidentiality and
anonymity was maintained.
Four validated and reliable tools were developed and three
standard tool used for data collection. Demographic
Proforma were used to collect information regarding demographic
characteristics, Standardised
perceived Stigma of Substance Abuse Scale (PSAS), Standardised Behavioural
problem Scale (BPS), Beck’s Depression Inventory.
Data was collected
through interview technique.
6. FINDINGS OF THE STUDY
6.1. Finding related to perceived stigma
The
current study found that, Majority 81% of substance abuse individual had
moderate perceived stigma whereas 18% had high perceived stigma and 1 % had low
perceived stigma. A study conducted by Belete Het al on “Perceived stigma and
associated factors among adults with problematic substance use in Northwest
Ethiopia” 36.1% had low-perceived stigma and the rest had high perceived
stigma. These findings fully supported with present study.
6.2. Finding related to behavioural problems
The current
study established that (85%) individuals with substance abuse were mild
behavioural problem and (15%) in individuals with substance abuse were moderate
behavioural problem.
A study conducted by Poudel A et al, on Psychosocial problems among individuals with substance use disorders in
drug rehabilitation centers, Nepal. The study focused on higher problems in substance use and
peer relationship domains while less in work adjustment domain though the score
were inconsistent.
6.3. Findings related to level of depression
The present review found that Most (41.5%)
individuals with substance abuse had moderate depression, (28%) had borderline
clinical depression, (27.5%) had mild mood disturbance, (3%) had these ups and
downs were considered normal.
Pradhan et al (2013) conducted a cross-sectional study on
depression among patients of substance use disorder. Among 42 subjects, 31
(73.8 %) were found to be suffering from Depression among which 19 (45.2%) had
mild to moderate depression and 12 (28.6%) had severe depression. This study partially supported with
present study.
In the present study, The
significant relation between perceived stigma and behavioural problems as the t
value is greater than table value 1.96 with df 198 at
0.05 level of significance. Study conducted by Latkin,2010 Strong relationship
between drug use stigma IV drug users and HIV risk behaviours p<.001.
7. DISCUSSION
The current
review found that, Majority 81% of substance abuse individual had moderate
perceived stigma whereas 18% had high perceived stigma and 1 % had low
perceived stigma. A study conducted by Belete Het al on “Perceived stigma and
associated factors among adults with problematic substance use in Northwest
Ethiopia” 36.1% had low-perceived stigma and the rest had high perceived
stigma. This findings complete supported with present
study.
Hadera et al. (2019) conducted a community-based cross-sectional survey was conducted at Bahir Dar town,
northwest Ethiopia cross-sectional study
design study on to assess the magnitude and associated factors of
perceived stigma among adults with mental illness in Ethiopia. A total of 384
participants were interviewed and the response rate was 100%. The prevalence of
high and low perceived stigma was 51% and 44%, respectively. This
findings partially supported with the present study.
The present
study found that (85%) individuals with substance abuse were mild behavioural
problem and (15%) in individuals with substance abuse were moderate behavioural
problem.
Strandheim A et al, The influence of behavioural and health problems on alcohol and
drug use in late adolescence - a follow up study of 2 399 young Norwegians Prospective population based cohort study of 2 399
adolescents attending the Young-HUNT study, aged 13-15 at baseline in 1995/97,
and 17-19 at follow-up 4 years later. At follow-up 19% of the students drank
alcohol once a week or more frequently.
This review uphold the opinion that especially
conduct problems.
The present
study found that Most (41.5%) individuals with substance abuse had moderate
depression, (28%) had borderline clinical depression, (27.5%) had mild mood
disturbance, (3%) had these ups and downs were considered normal.
Pradhan et al (2013) conducted a
cross-sectional study on depression among patients of substance use disorder.
Among 42 subjects, 31 (73.8 %) were found to be suffering from Depression among
which 19 (45.2%) had mild to moderate depression and 12 (28.6%) had severe
depression. This study partially supported with present study.
In the present study, The significant relation between perceived stigma and
behavioural problems as the t value is greater than table value 1.96 with df 198 at 0.05 level of significance. Study conducted by
Latkin,2010 Strong relationship between drug use stigma IV drug users and HIV
risk behaviours p<.001.
In the present study statistically
significant association between level of depression with selected demographic variables
(Regularity of treatment) as the calculated value of chi square is greater than
table value of chi square at 0.05 level of significance. Study conducted by
Luoma,2010 The measure of perceived stigma was significantly associated with
internalized stigma p<00001. this was fully supported with present study.
8. CONCLUSION
Based on the findings of the present study, it can be concluded that majority of the people average perceived stigma followed by greater perceived stigma & lesser perceived stigma. In the domain i.e. highest mean% of behavioural externalising problems and internalising behavioural problems. Majority of individuals had moderate depression followed by borderline clinical depression, mild mood disturbance and these ups and downs were considered normal. There is statistically significant association between level of depression with selected demographic variables (Regularity of treatment). There was a positive relation between perceived stigma & Behavioural problem individuals with substance abuse
9. LIMITATION
The study has several limitations.
The outcome
of this study shall not be universal to apply to the county wide. The study
with its boundary is only 200 sample a general analysis carried out on
de-addiction center. Consequently, other
investigations on the same topic can be reproduced in other counties. The study
subjects are limited to few settings.
10. RESULTS
Computed data are organized and presented under various subheadings according to objectives of the study.
10.1. Demographic characteristics
Table 1
|
Table 1 Frequency & Percentage Distribution of Demographic Characteristics of Individual with Substance Abuse |
||
|
Category |
Frequency |
Percentage (%) |
|
Age (in years) |
||
|
18-26 |
30 |
15 |
|
27-34 |
69 |
34.5 |
|
35-42 |
61 |
30.5 |
|
43-50 |
40 |
20 |
|
Educational status |
||
|
No formal education |
33 |
16.5 |
|
Primary |
75 |
37.5 |
|
Secondary |
68 |
34 |
|
Higher secondary |
20 |
10 |
|
Graduate &above |
4 |
2 |
|
Occupation |
||
|
Unemployed |
49 |
24.5 |
|
Independent business |
95 |
47.5 |
|
Government service |
35 |
17.5 |
|
Private job |
21 |
10.5 |
|
Marital status |
||
|
Unmarried |
87 |
43.5 |
|
Married |
113 |
56.5 |
|
Family Type |
||
|
Nuclear |
117 |
58.5 |
|
Joint |
83 |
41.5 |
|
Residence |
||
|
Rural |
81 |
40.5 |
|
Urban |
119 |
59.5 |
|
Family History of substance abuse |
||
|
Yes |
71 |
35.5 |
|
No |
129 |
64.5 |
|
Types of substance abuse |
||
|
Alcohol |
42 |
21 |
|
Marijuana |
51 |
25.5 |
|
Vaping |
51 |
25.5 |
|
Illicit drug |
56 |
28 |
|
Duration of substance use |
||
|
1-5
yrs |
83 |
41.5 |
|
6-10 yrs |
117 |
58.5 |
|
Co- addictor of substance
abuse |
||
|
Own |
64 |
32 |
|
Friend |
130 |
65 |
|
Relatives |
6 |
3 |
|
Regularity of treatment |
||
|
Yes |
97 |
48.5 |
|
No |
103 |
51.5 |
Figure 1
|
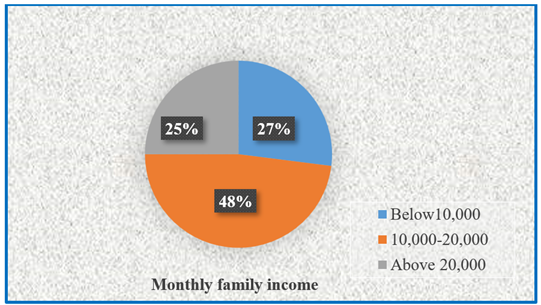
Figure 1 Pie Chart Showing Frequency and Percentage Distribution of Monthly Family Income Among Individuals with Substance Abuse. 48% Belonged to Monthly Family Income Rs. 10,000-20,000, 27% Belonged to Rs. Below 10,000 and 25% Belonged to Rs. Above 20,000. Among Individuals with Substance Abuse. |
Table 2
|
Table 2 Frequency & Percentage Distribution of Perceived Stigma Among Individuals with Substance Abuse n=200 |
||
|
Perceived stigma |
Frequency |
Percentage (%) |
|
Low (< 19) |
2 |
1 |
|
Moderate (19-26) |
162 |
81 |
|
High (>26) |
36 |
18 |
Table 2 shows that majority
81% individual with substance
abuse had moderate perceived stigma whereas 18% had
high perceived stigma and 1% had low perceived stigma.
Table 3
|
Table 3 Frequency & Percentage Distribution of Behavioural Problem Among Individuals with Substance Abuse n=200 |
||
|
Behavioural problem |
Frequency |
Percentage (%) |
|
Mild (< 30) |
170 |
85 |
|
Moderate (30-40) |
30 |
15 |
|
Severe (>40) |
Nil |
__ |
Table 3 shows that (85%) individuals with substance abuse were mild behavioural problem and (15%) among individuals with substance abuse were moderate behavioral problem.
Table 4
|
Table 4 Domain Wise Behavioral Problem of Among Individuals with Substance Abuse
n=200 |
|||||
|
Domain Rank |
Score range |
Max. score |
Min. score |
Mean |
Mean% |
|
Externalising |
|||||
|
Problems 1 |
5 – 25 |
16 |
7 |
11.32 |
45.3 |
|
Intranalising |
|||||
|
Problems 2 |
May-25 |
14 |
7 |
10.2 |
40.3 |
Table 4 shows that heighest
mean% of behavioural externalising
problems score was 45.3% and lowest mean% of internalizing behavioural
problems score was 40.3%.
Table 5
|
Table 5 Frequency & Percentage Distribution of Level of Depression Among Individuals with Substance Abuse n=200 |
||
|
Score range Level of depression |
Frequency |
Percentage (%) |
|
1-10_These ups and downs are
considered normal |
6 |
3 |
|
11-16__Mild mood disturbance |
55 |
27.5 |
|
17-20 __Borderline clinical depression |
56 |
28 |
|
21-30__Moderate depression |
83 |
41.5 |
|
31-40__Severe depression |
Nil |
__ |
|
Over40__Extreme depression |
Nil |
__ |
Table 5 shows that (41.5%) individuals had mmoderate depression, (28%) had bborderline clinical depression, (27.5%) had mild mood disturbance, (3%) had these ups and downs were considered normal.
Table 6
|
Table 6 Area- Wise Rank Order of Level of Depression Score Among Individuals with Substance Abuse n=200 |
|||||
|
S. No. |
Area |
Maximum possible score |
Obtain mean score |
Mean percentage |
Rank Order |
|
1 |
Sadness |
3 |
0.55 |
18.33 |
20 |
|
2 |
Pessimism |
3 |
0.545 |
18.17 |
21 |
|
3 |
Part failure |
3 |
0.695 |
23.17 |
19 |
|
4 |
Loss of pressure |
3 |
0.96 |
32 |
5 |
|
5 |
Guilty feeling |
3 |
1.16 |
38.67 |
1 |
|
6 |
Punishment feeling |
3 |
0.90 |
30 |
15 |
|
7 |
Self -dislike |
3 |
0.85 |
28.33 |
16 |
|
8 |
Self -criticalness |
3 |
0.95 |
31.67 |
7 |
|
9 |
Suicidal thought or wishes |
3 |
1 |
33.33 |
2 |
|
10 |
Crying |
3 |
0.834 |
27.8 |
18 |
|
11 |
Agitation |
3 |
0.84 |
28 |
17 |
|
12 |
Loss of interest |
3 |
0.975 |
32.5 |
4 |
|
13 |
Indecisiveness |
3 |
0.99 |
33 |
3 |
|
14 |
Worthlessness |
3 |
0.942 |
31.4 |
9 |
|
15 |
Loss of energy |
3 |
0.925 |
30.83 |
12 |
|
16 |
Change in sleeping Pattern |
3 |
0.915 |
30.5 |
13 |
|
17 |
Irritability |
3 |
0.945 |
31.5 |
8 |
|
18 |
Change in appetite |
3 |
0.91 |
30.33 |
14 |
|
19 |
Concentration dificulty |
3 |
0.955 |
31.83 |
6 |
|
20 |
Tiredness or fatique |
3 |
0.935 |
31.17 |
11 |
|
21 |
Loss of interest in sex |
3 |
0.940 |
31.33 |
10 |
Table 6 shows that maximum possible score,
obtained mean, mean% and rank order of 21 items questionnaire of Beck’s
depression inventry response given by the individuals
with substance abuse. The highest mean % (38.67) individuals with substance
abuse guilty feeling of level of depression and lowest mean % (18.17) pessimism
of level of depression.
Table 7
|
Table 7 Relationship Between Perceived Stigma with Behavioural Problem Among Individuals with Substance Abuse n=200 |
|||||
|
Variable |
Mean |
Median |
Corr. Coeff (r) |
t value |
P.value |
|
Perceived stigma |
24.74 |
25 |
0.162 |
2.31 |
.021 |
|
Behavioural problem |
21.52 |
22 |
|||
Table 7 shows that there
was a week positive
relation between perceived stigma &Behavioural problem as the correlation
between them is 0.162& P.
value is. 021. There is statistically significant
relation at 0.05 level of significance.
Table 8
|
Table 8 Relationship Between Perceived Stigma with Depression Among Individuals with Substance Abuse n=200 |
|||||
|
Variable |
Mean |
Median |
Corr. Coeff (r) |
t value |
P.value |
|
Perceived stigma |
24.74 |
25 |
-0.138 |
1.96 |
.051 |
|
Depression |
18.76 |
19.50 |
|||
Table 8 shows that there
was a negative relation
between perceived stigma & depression as the correlation between them is
-0.138 at 198 degree of freedom, where the calculated values 1.96 & P.
value is. 051. So we can infer that if the perceived
stigma is low then depression level will be low.
Table 9
|
Table 9 Relationship Between Behavioural Problem with Depression Among Individuals with Substance Abuse n=200 |
||||||
|
Variable |
Mean |
SD |
Median |
Corr. Coeff (r) |
t. value |
P. value |
|
Behavioural problem |
21.52 |
2.718 |
22 |
-0.085 |
1.20 |
.231 |
|
Depression |
18.76 |
4.234 |
19.50 |
|||
Table 9 shows that there is a
negative relation between perceived stigma & Behavioural problem as the
correlation between them is -0.085 at 198 degree of freedom, where the calculated
values 1.20 is less than the table value & P. value is. 231. So we can infer that if the behavioural problem is low then
depression level will be low.
Table 10
|
Table 10 Association Between Perceived Stigma with Selected Demographic Variables
n=200 |
|||||
|
Category |
Stigma |
X2 |
DF |
P. Value |
|
|
< median |
≥ median |
||||
|
Age (in years) |
|||||
|
18-26 |
14 |
16 |
2.649 |
3 |
.448 |
|
0.448 |
29 |
40 |
|||
|
27-34 |
20 |
41 |
|||
|
35-42 |
13 |
27 |
|||
|
43-50 |
|||||
|
Educational status |
|||||
|
No formal education |
12 |
21 |
2.496 |
4 |
.645 |
|
Primary |
29 |
46 |
|||
|
Secondary |
25 |
43 |
|||
|
Higher secondary |
7 |
13 |
|||
|
Graduate &above |
3 |
1 |
|||
|
Occupation |
|||||
|
Unemployed |
20 |
29 |
2.421 |
3 |
.489 |
|
Independent buiseness |
31 |
64 |
|||
|
Government service |
16 |
19 |
|||
|
Private job |
9 |
12 |
|||
|
Marital status |
|||||
|
Unmarried |
35 |
51 |
0.584 |
1 |
.444 |
|
Married |
40 |
73 |
|||
|
Family Type |
|||||
|
Nuclear |
43 |
74 |
0.186 |
1 |
.666 |
|
Joint |
33 |
50 |
|||
|
Monthly family income |
|||||
|
Below Rs 10,000 |
20 |
34 |
0.642 |
2 |
.725 |
|
Rs 10,000-20,000 |
39 |
57 |
|||
|
Above Rs 20,000 |
17 |
33 |
|||
|
Residence |
|||||
|
Urban |
43 |
76 |
0.434 |
1 |
0.510 |
|
Rural |
33 |
48 |
|||
|
Types of substance abuse |
|||||
|
Alcohol |
21 |
21 |
7.673 |
3 |
.053 |
|
Marijuana |
19 |
32 |
|
|
|
|
Opioids |
12 |
39 |
|
|
|
|
Illicit
drug |
24 |
32 |
|
|
|
|
Duration of substance use |
|||||
|
1-5 yrs |
33 |
50 |
0.186 |
1 |
.666 |
|
6-10 yrs |
43 |
74 |
|
|
|
|
Co-addictor
of substance abuse |
|||||
|
Own |
22 |
42 |
0.807 |
2 |
.667 |
|
Friend |
51 |
79 |
|
|
|
|
Relatives |
3 |
|
|
|
|
|
Regularity of treatment |
|||||
|
Yes |
41 |
56 |
1.456 |
1 |
.227 |
|
No |
35 |
68 |
|
|
|
Table 10 shows that there are no statistically strong relation between perceived stigma with selected demographic variables as the calculated value of chi square is lower than table value of chi square at 0.05 level of significance.
Table 11
|
Table 11 Association Between Level of Depression with Selected Demographic Variables
n=200 |
|||||
|
Category |
Level of depression |
X2 |
DF |
P. Value |
|
|
< median |
≥ median |
||||
|
Age (in years) |
|||||
|
18-26 |
11 |
19 |
2.912 |
.405 |
|
|
27-34 |
37 |
32 |
|||
|
35-42 |
30 |
31 |
|||
|
43-50 |
22 |
18 |
|||
|
Educational status |
|||||
|
No formal education |
14 |
19 |
2.630 |
4 |
.621 |
|
Primary |
38 |
37 |
|||
|
Secondary |
33 |
35 |
|||
|
Higher secondary |
12 |
8 |
|||
|
Graduate &above |
3 |
1 |
|||
|
Occupation |
|||||
|
Unemployed |
24 |
28 |
0.877 |
3 |
.830 |
|
Independent business |
46 |
49 |
|||
|
Government service |
20 |
15 |
|||
|
Private job |
10 |
11 |
|||
|
Marital status |
|||||
|
Unmarried |
43 |
43 |
0.004 |
1 |
.949 |
|
Married |
57 |
56 |
|||
|
Family Type |
|||||
|
Nuclear |
54 |
63 |
1.166 |
1 |
.666 |
|
Joint |
46 |
37 |
|||
|
Monthly family income |
|||||
|
BelowRs 10,000 |
31 |
23 |
2.646 |
2 |
.266 |
|
Rs 10,000-20,000 |
48 |
48 |
|||
|
AboveRs 20,000 |
21 |
29 |
|||
|
Residence |
|||||
|
Urban |
41 |
40 |
0.021 |
1 |
.884 |
|
Rural |
59 |
60 |
|
|
|
|
Family history of substance
abuse |
|||||
|
Yes |
36 |
35 |
0.022 |
1 |
.882 |
|
No |
64 |
65 |
|
|
|
|
Types of substance abuse |
|||||
|
Alcohol |
20 |
22 |
0.291 |
2 |
.864 |
|
Marijuana |
25 |
26 |
|
|
|
|
Opioids |
27 |
24 |
|
|
|
|
Illicit
drug |
28 |
28 |
|
|
|
|
Duration of substance use |
|||||
|
1-5 yrs |
45 |
38 |
1.009 |
1 |
.315 |
|
6-10 yrs |
55 |
62 |
|
|
|
|
Co-addictor
of substance abuse |
|||||
|
Own |
34 |
30 |
1.194 |
2 |
.550 |
|
Friend |
62 |
68 |
|
|
|
|
Relatives |
4 |
2 |
|
|
|
|
Regularity of treatment |
|||||
|
Yes |
57 |
40 |
4.541 |
1 |
.033 |
|
No |
45 |
58 |
|
|
|
Table 11 shows that there is consequential association between level of depression with Regularity of treatment as the calculated value of chi square is greater than table value of chi square at 0.05 level of significance.
CONFLICT OF INTERESTS
None.
ACKNOWLEDGMENTS
None.
REFERENCES
Fiato, R. (2005). Domestic Violence and Alcohol Abuse: Couples Therapy Treatment Programs. State
University of New York Empire State College.
Great Britain (2010, Jul 2). Department of Health, Great Britain. Parliament. House of Commons. Tackling Inequalities in Life Expectancy in Areas with the Worst Health and Deprivation: Department of Health. The Stationery Office.
Hadera, E., Salelew, E., Girma, E., Dehning, S., Adorjan, K., & Tesfaye, M. (2019, Mar 27). Magnitude and Associated Factors of Perceived Stigma Among Adults with Mental Illness in Ethiopia. Psychiatry Journal. https://doi.org/10.1155/2019/8427561
Kulesza, M., Larimer, M.E., & Rao, D. (2013, May 1). Substance use Related Stigma: What we Know and the Way Forward. Journal of Addictive Behaviors, Therapy & Rehabilitation, 2(2). https://doi.org/10.4172/2324-9005.1000106
Luoma, J.B., Chwyl, C., Bathje, G.J., Davis, A.K., & Lancelotta, R. A. (2020, Aug 7). Meta-Analysis of Placebo-Controlled Trials of Psychedelic-Assisted Therapy. Journal of Psychoactive Drugs, 52(4), 289-99. https://doi.org/10.1080/02791072.2020.1769878
Luoma, J.B., Martin, C.E., & Pearson, J.L. (2002, Jun 1). Contact with Mental Health and Primary Care Providers Before Suicide: A Review of the Evidence. American Journal of Psychiatry, 159(6), 909-16. https://doi.org/10.1176/appi.ajp.159.6.909
Sidana, A., Walia, N., Jaswal, S. (2021). Ten Years Outcome of In-Patient with Substance use Disorder-A Study from North India, 245-252.
World Health Organization (1994). Lexicon of Alcohol and Drug Terms. Inlexicon of Alcohol and Drug Terms.
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© Granthaalayah 2014-2024. All Rights Reserved.