
Survey on biomaterial shrilk as sutures in medical field
Sonaali Borkar 1![]()
![]() ,
Pratik Vetal 2
,
Pratik Vetal 2![]()
![]()
1 Assistant
Professor, Department of Applied Science, Wadala, Mumbai, India
2 Student,
Department of Biomedical Engineering, Wadala, Mumbai, India
|
|
ABSTRACT |
||
|
Shrilk stands as an innovative
biomaterial, fusing the robustness of chitosan, a synthetic plastic, with the
resilience of shrimp shells. The term "shrilk"
itself is a blend of "shrimp" and "silk," emblematic of
the distinctive attributes inherent in this material. Chitosan, derived from
chitin present in the exoskeletons of crustaceans like shrimps and crabs,
boasts biocompatibility, biodegradability, and antimicrobial qualities.
Biopolymers have garnered increased attention owing to their remarkable
attributes such as biocompatibility, biodegradability, non-toxicity, and
functionality. These characteristics position biopolymers as promising
candidates for a wide range of surgical applications, including but not
limited to bioadhesives, sealants, sutures, and
wound dressings. Dubbed "shrilk" by its
creators, Postdoctoral fellow Javier Fernandez and Wyss Institute director
Donald Ingber, this substance mimics insect cuticle, a material found in
insect exoskeletons. Shrilk serves as the synthetic
equivalent to one of nature's most robust, lightweight, and intriguing
materials. This article underscores the potential use of shrilk
in surgical applications, particularly as sutures, considering its properties
in comparison to currently employed sutures. |
|||
|
Received 10 February
2024 Accepted 10 March 2024 Published 31 March 2024 Corresponding Author Sonaali Borkar, sonaali.borkar@vit.edu.in DOI 10.29121/granthaalayah.v12.i3.2024.5517 Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2024 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
Keywords: Shrilk, Sutures,
Biomaterial |
|||
1. INTRODUCTION
Sutures, commonly referred to as stitches, serve as medical instruments employed to secure the edges of wounds or surgical incisions, fostering the healing process. They find widespread application in diverse medical procedures, including surgeries, wound closures, and various interventions. Two primary categories classify sutures: Absorbable sutures and Non-Absorbable sutures. An ideal suture is characterized by qualities such as resistance to unexpected breakage during application, minimal elongation in response to wound edema, biocompatibility, ease of handling, capability to form secure knots, and, if utilized internally, a capacity to biodegrade within an appropriate timeframe. Selecting an appropriate suture material for wound closure and healing requires careful consideration of several crucial parameters. Commonly utilized suture materials include Dexon (polyglycolic acid), Vicryl (copolymer of glycolide and lactide), surgical silk, Nurolon (Nylon 66), Ethilon (Nylon 66), Mersilene (polyester), and Prolene (polypropylene). Each of these materials possesses unique characteristics that make them suitable for specific medical applications. When choosing a suture material for wound closure and healing, it is crucial to take into account important factors such as suture resistance, tissue retention capacity, absorbency, the risk of infection, and the potential inflammatory response induced by the suture material. These elements are pivotal in guaranteeing successful wound closure and fostering optimal healing results.. There are many complications with the currently used sutures, and they vary depending upon the type of suture material used. Following an extensive surgery that spans several hours, wound care may not be the immediate focus for the medical team. Nevertheless, the success of even the most intricate surgery can be jeopardized if the wound closure is not meticulously executed. The term for the unraveling of a suture and subsequent separation of wound edges is known as wound dehiscence. Ensuring proper stitching during the closure phase is crucial for the overall success of the surgical procedure. By reinforcing chitosan with fibers from shrimp shells, researchers have developed a material that exhibits exceptional strength, toughness, and flexibility. Shrilk has attracted significant attention in various fields due to its potential applications. Its exceptional strength, lightweight nature, and biodegradability make it suitable for use in environmentally friendly packaging materials, biomedical implant, drug delivery systems and in structural components for aerospace engineering. Shrilk's components have received approval from the Food and Drug Administration (FDA), enhancing its potential for medical applications.. It shows promise as a potential material for sutures in medical field due to its specific properties it is an attractive candidate for this application.
2. LITERATURE SURVEY
When selecting an appropriate suture material for wound closure and healing, a comprehensive consideration of several pivotal parameters is imperative. These factors encompass suture resistance, tissue-retention capacity, absorbency, risk of infection, and the inflammatory response induced by the chosen suture material. This meticulous evaluation ensures the optimal choice for specific medical applications, contributing to successful wound closure and healing outcomes. Non-absorbable sutures find frequent use in the closure of external wounds, typically necessitating removal through a secondary operation. In contrast, absorbable sutures offer versatility, proving effective for both internal and external wound closure, eliminating the need for subsequent removal procedures. The historical suture material, catgut, while the oldest natural and degradable option, faced challenges a few years post-introduction. It became associated with hypersensitivity reactions and an elevated incidence of infections, leading many surgeons to eschew its use and attribute complications to catgut sutures. Silk emerges as a prominent choice among natural non-absorbable suture materials, boasting various advantages such as excellent tissue compatibility, high suppleness, easy handling, and knot strength. However, the utilization of silk presents a notable challenge due to its vulnerability to microbial attacks and mechanical properties that can potentially hinder the optimal progression of wound healing. In the realm of suture material selection, navigating the delicate balance between advantageous features and potential drawbacks is paramount. This nuanced approach ensures that the chosen suture material aligns seamlessly with the specific requirements of diverse medical scenarios, contributing to the success of surgical interventions and postoperative recovery Bibire et al. (2022). Prominent instances of biomedical applications leveraging biopolymers encompass an array of innovative and life-enhancing technologies. These include, but are not limited to, soft-tissue replacement vascular grafts, breast implants, intraocular lenses, artificial hearts, components integral to extracorporeal oxygenators, contact lenses, plasmapheresis units, sutures, adhesives, blood substitutes, dialyzers, bone cement, artificial skin, and drug delivery systems strategically targeting sites of tumors or inflammation. This diverse spectrum of biomedical applications underscores the versatile and transformative nature of biopolymers in advancing medical interventions for improved patient outcomes and enhanced quality of life Meril Life Sciences Pvt. Ltd. (n.d.).
The primary distinction that sets biopolymers apart from their synthetic counterparts lies in their unparalleled biocompatibility. While biopolymers boast a structurally intricate yet well-defined composition, they stand out for their inherent functional properties, as well as their remarkable characteristics of degradability and renewability. Noteworthy biopolymers used in surgical materials include chitosan, alginate, and hyaluronic acid as polysaccharides; collagen, gelatin, and fibroin as proteins; and various biocompatible polymers derived from polylactic acid derivatives. Despite these remarkable advantages, biopolymers are not without their challenges. They may exhibit inferior mechanical properties, reduced productivity, and a degree of susceptibility to environmental factors. However, strategic functionalization approaches have demonstrated the potential to substantially enhance their properties, mitigating some of these limitations. This nuanced balance between advantages and challenges underscores the ongoing quest for refining and optimizing the utilization of biopolymers in surgical applications, marking a significant stride towards the convergence of cutting-edge biomedical technology with nature's intricate designs. Shrilk is a combination of two natural polymers chitosan and fibroin. It exhibits the properties of both the natural polymers i.e. biocompatibility, biodegradability, antimicrobial properties, hemostatic properties (can promote blood clotting and help control bleeding), film-forming ability, Regenerative properties. The Shrilk laminate demonstrates an impressive ultimate strength of 119 MPa, surpassing previous descriptions of a chitosan-fibroin blend with similar weight ratios by a factor of ten. Notably, Shrilk exhibits double the strength of its strongest component, chitosan, and displays unique properties in comparison to other high-strength materials. Its strength is twice that of nylon or polylactic acid (PLA), and it rivals aluminum alloys in strength while weighing only half as much due to its lower density. In terms of water absorption, chitosan outperforms fibroin, absorbing water over twice as efficiently. Quantitative analysis of water absorption by Shrilk films, through a comparison of dry and water-saturated samples, revealed independent water uptake by the fibroin and chitosan layers along with their interface. Despite a reduction in strength to approximately 3.5 MPa when saturated with water—more than thirty times below its dry state strength—the material retained impressive energy absorption before breakage, only experiencing a marginal decrease by a factor of two. The remaining energy seemed to be stored as an increase in the material's elasticity, supporting up to 23% ultimate strain, nearly ten times higher than what Shrilk can bear in a dry state. This configuration positions Shrilk as a potential biocompatible and biodegradable scaffold, particularly for applications such as small vessel repair or nerve conduits due to its high compatibility. The strong affinity between chitosan and fibroin layers, along with the composite's stability against water, enables the joining of multiple Shrilk laminates by "gluing" them with fibroin. This innovative approach allows for the creation of thicker, stronger, and more intricate structures tailored for specialized applications. Fernandez & Ingber (2012).
3. BACKGROUND
Shrilk in a derivate of chitosan and fibroin derived from shrimp shells and silk.
1) Chitosan
Chitosan, derived from marine animals, is a highly biocompatible, non-toxic, and biodegradable polymer with antimicrobial properties. Its cationic nature contributes to these properties, and it exhibits good absorbability, permeability, and moisture retention. Chitosan sutures, crafted from chitin, showcase impressive mechanical strength while maintaining a notable absence of allergic reactions or inflammation. While its low mechanical strength limits its use, it is commonly employed as a coating for sutures. In the biomedical field, chitosan is utilized in bandages and sutures for wound healing due to its tough, oxygen-permeable, water-absorbent, and biocompatible film. Additionally, its high oxygen permeability makes it suitable for contact and intraocular lenses. It can also be applied directly as an aqueous solution to treat burns.
Figure 1
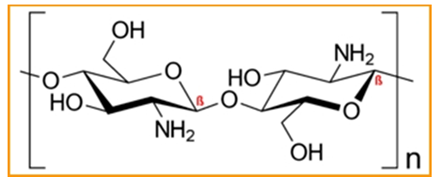
|
Figure 1 Structure of Chitosan |
2) Fibroin
Silk fibroin, derived from the Bombyx mori silkworm, stands as a time-honored fiber with a rich history spanning centuries., was initially proposed for surgical sutures due to its slow degradation, good mechanical strength, and excellent biocompatibility. Despite being preferred for cardiovascular, neurological, and ophthalmic procedures, its high inflammatory reactions and susceptibility to bacterial colonization around suture knots pose challenges. To tackle this issue, researchers propose various strategies, including the incorporation of antibiotics, nanoparticles, and biomaterials. Silk sutures infused with antibiotics have demonstrated efficacy in preventing bacterial adherence and biofilm formation, thereby augmenting the overall functionality of silk sutures.
Figure 2
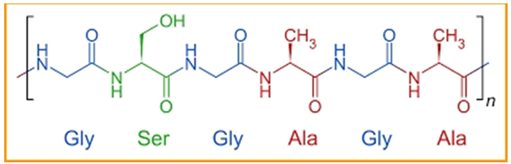
|
Figure 2 Structure of Fibroin |
3) Silk
Sutures
Silk suture, crafted from Fibroin, an organic protein, is a non-absorbable surgical suture. Colored black for visibility and braided for ease of handling, it finds application in cardiovascular, ophthalmic, and neurological surgeries. Despite being prone to bacterial growth due to its natural origin, it is utilized for soft tissue approximation. While having the lowest tensile strength among available sutures, its softness makes it suitable for temporary use during surgery. Remarkably, it retains 50% of its tensile strength even after a year.
4) Chitin
Sutures
Chitin sutures offer an organic alternative with prolonged mechanical properties. Derived from glucose in arthropods and crustaceans, chitin sutures demonstrate minimal adverse reactions during tissue exposure. Improved through research, these sutures maintain tensile strength, Young modulus, and flexibility longer than alternatives like catgut and Dexon. Reinforcement with cellulose nanocrystals enhances their physical properties. Fully biodegradable and biocompatible, chitin sutures promote cell regeneration, accelerating wound healing without the need for antibiotics to reduce infection risk.
·
Material Fabrication
To fabricate Shrilk, an initial step involved the formation of a chitosan film, which was then dried on a petri dish according to the specified method. Subsequently, a fibroin solution was cast onto this chitosan layer and allowed to dry at 37°C for a duration of 12 hours. The resulting laminate underwent immersion in methanol for 30 minutes to induce the beta (insoluble) transition of the protein. Following this, a thorough washing with deionized water and subsequent drying were carried out. For the construction of more robust, multilayer structures, several Shrilk films were stacked together, with a modest amount of fibroin solution applied between each layer. The removal of trapped bubbles was achieved through physical compression of the materials using a microscope slide. The final steps involved water evaporation at 37°C and a methanol treatment to induce the beta transition of the new fibroin within the multilayered structure.
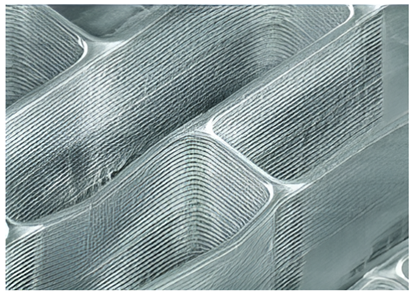
Figure 3

|
Figure 3 Biomaterial Shrilk |
4. NOVELTY
Shrilk, an innovative biomaterial derived from natural sources, offers several advantages over traditional synthetic sutures. Its enhanced biocompatibility reduces the risk of adverse reactions and tissue irritation, promoting improved patient comfort during the healing process. Unlike synthetic sutures that require a separate removal procedure, Shrilk sutures biodegrade within the body, eliminating the need for suture removal and minimizing patient discomfort and infection risks. One of Shrilk's key components, chitosan, imparts antimicrobial properties, further enhancing its suitability for sutures. This antimicrobial activity may help reduce the risk of surgical site infections when Shrilk sutures are used. Researchers have also highlighted Shrilk's cost-effectiveness and ease of large-scale production, making it an environmentally friendly option that does not require land use, unlike plant-based bioplastics. When discarded, Shrilk breaks down within weeks, releasing nutrients that support plant growth. Its versatility allows for the creation of diverse 3D forms with impressive precision, as noted by Fernandez, a researcher involved in its development. Moreover, researchers have demonstrated the ability to control stiffness variations by adjusting water content during the fabrication process, balancing strength, and elasticity. Overall, Shrilk presents a promising alternative to synthetic plastics, with potential applications in everyday items such as trash bags and toy packaging, offering a sustainable and biocompatible solution for various medical and environmental challenges.
1) Complications
with sutures
The concluding step in a surgical procedure involves the closure of the wound, a process that falls into two main categories: primary closure and secondary closure. Primary closure entails the use of sutures to tightly seal the skin, facilitating direct and prompt wound healing. Conversely, in secondary closure, the deliberate decision is made to leave the wound open, allowing it to undergo healing through the natural mechanisms of granulation and contraction. Proper stitching during closure is crucial, as a suture coming undone can lead to wound dehiscence. Causes include:
• Excessive tension
• Foreign objects or infection
• Incorrect knots or technique
• Sutures placed too close to the wound edge
• Loose knots
• Incorrect materials
• Blood clot formation.
Symptoms associated with a dehisced wound include noticeable signs such as the breakage of sutures, the widening of the wound, pain, swelling, discharge of pus, bleeding, frothy drainage, and the onset of fever. These indicators can be particularly pronounced in individuals with excess weight or diabetes, potentially leading to heightened vulnerability to arterial bleeding. Complications associated with sutures include infection, inflammation, allergic reactions to materials like silk or nylon, delayed healing, excessive scarring, suture granulomas, suture breakage under tension, suture abscess formation, tissue reactions causing discomfort, and permanent marks or indentations on the skin. These risks highlight the importance of proper wound care and choice of suture materials.
2) Objective
All the commonly used suture material lack some or the other property, while Shrilk exhibits mechanical properties comparable to or even surpassing those of traditional synthetic sutures. It is biocompatible, well-tolerated by the human body, and resistant to mechanical stress due to its combination of strength and toughness. Shrilk is biodegradable, gradually breaking down as the wound heals, eliminating the need for suture removal. Its flexibility makes it easy for surgeons to handle and tie knots, while its anti-inflammatory properties reduce irritation at the suture site. The material offers a customizable degradation rate and can be transparent for improved visualization during surgery. Shrilk can also be tailored for bioadhesive properties, enhancing tissue adherence, and minimizing the risk of complications. Nevertheless, it's important to note that its clinical use may vary, and it should undergo rigorous testing and regulatory approvals before widespread application in medical practice.
Table 1
|
Table 1 Comparison Between Six Commonly Used Suture Material and Shrilk of Various Properties Necessary for an Ideal Suture |
|||||||
|
Suture
Materials |
Dexon (poly-glycolylic
acid) |
Vicryl (copolymer of glycolide and lactide) |
Nurolon (nylon 6,6) |
Ethilon (Nylon 6,6) |
Mersilene (Polyester) |
Prolene (Propylene) |
Shrilk (chitosan: fibroin) 1:2 |
|
Breaking
Strain (%) |
22.6 (26.3) |
18.4 (20.8) |
18.2 (21) |
33 (37) |
8 (8.2) |
42 (43.2) |
Fibroin 10-15% Chitosan 2-10% |
|
Tensile
Strength (MPa) |
56 |
32 |
75.3 |
75.3 |
- |
44 |
119 |
|
Modulus
of Elasticity (N/Tex or GPa) |
6.63 |
5.46 |
1.32 |
2.8 |
8.96 |
14.69 |
Chitosan - 4.7 Fibroin - 10 |
|
Melting
Point (OC) |
>200 |
150-175 |
268.8 |
268.8 |
140-185 |
-185.2 |
Chitosan 215-217 Fibroin 238-287 |
|
Allergenicity |
No |
No |
No |
No |
No |
Yes [6] |
No |
|
Absorbable
or non-absorbable |
Absorbable |
Absorbable |
Non- Absorbable |
Non- Absorbable |
Non- Absorbable |
Non - Absorbable |
Non- Absorbable |
|
Water
Resistance |
- |
No |
No |
No |
No |
No |
No |
Figure 4
|
Figure 4 Highly Maginified View of Micropatterned Surface Topography of the Fibroin Covering Layer of Shrilk is Showcased, Featuring Tightly Packed Rectangular Lacunae Generated Through a Micromolding Technique (Scale Bar, 50 μm) |
Figure 5
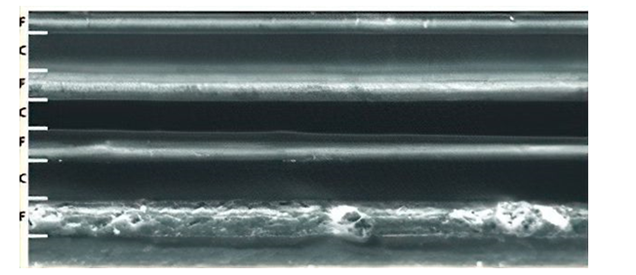
|
Figure 5 A Scanning Electron Microscopy Image that Displays a Cross-Sectional View of Microfabricated Multi-Laminate Material, Showcasing the Intricacies of Design. |
Figure 6
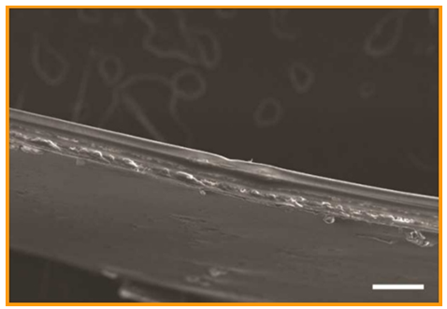
|
Figure 6 A Scanning Electron Micrograph Depicting the Cross-Sectional View of a Microfabricated Multi-Laminate Shrilk Structure. |
Figure 7
|
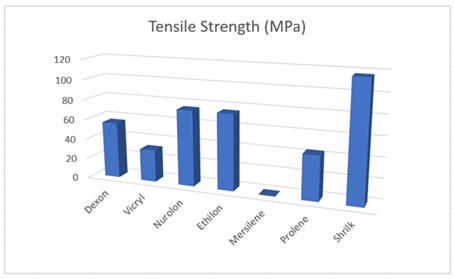
Figure 7 Graph of Tensile Strength (MPa) of Commonly Used Sutures Materials and Shrilk |
Figure 8
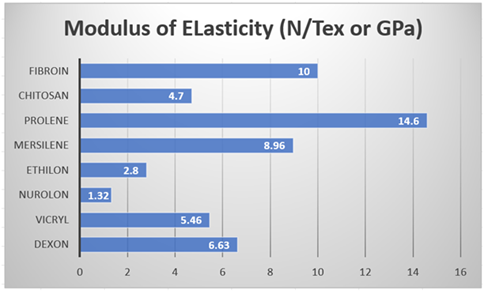
|
Figure 8 Graphical Representation of Modulus of Elasticity (N/Tex or GPa) of Commonly Used Suture Materials. |
5. RESULTS AND DISCUSSION
While choosing an appropriate material for the suture several properties are considered like Tensile strength or breaking strain is the weight necessary to break a suture divided by the cross-sectional area of the suture Dart & Dart (2011). This property prevents premature breakage, supports tissue healing, and minimizes trauma. Sutures with sufficient tensile strength are durable and can accommodate tissue swelling, contributing to effective wound closure. From Table 1 shrilk exhibits higher tensile strength as well as breaking strain than all the other suture materials considered. Another property that is considered while choosing suture material is elasticity, it is the ability of a suture material to adapt to changing tissues. The elastic property of material prevents knot loosening and damage to tissue margins under shear. Comparatively the information about elasticity is not available, considering those of its ingredients i.e chitosan and fibroin, chitosan shows less elasticity and fibroin shows more elasticity on comparison with other suture materials. Melting point also plays a crucial role as it determines at what temperature the suture material will lose its structural integrity and potentially degrade. For absorbable sutures, which are designed to break down in the body over time, the melting point is crucial because it signifies the point at which the material will be absorbed. This property ensures that the suture degrades at an appropriate rate, aligning with the healing process and minimizing the risk of long-term complications. For non-absorbable sutures, a high melting point is important to ensure stability and prevent unintended breakdown or deformation during sterilization procedures or in the body. Chitosan and fibroin possess high melting point making shrilk a non-absorbable material, but on the other hand it shows biodegradability. According to its researchers, shrilk is biodegradable, it can dissolve in human body as well as being a non-absorbable material it can be used for external wound covering. While Shrilk presents numerous potential applications and advantages, certain challenges have been identified. One notable concern is Shrilk's sensitivity to moisture, which can impact both its stability and toughness. The material is susceptible to hydrolysis, leading to decomposition in the presence of water. Nevertheless, addressing this issue is possible through material modification, such as the addition of cross-linking agents or other additives. These modifications have the potential to enhance Shrilk's mechanical properties and increase its resistance to hydrolysis, warranting further research in this area. Another approach can be developing new processing methods. Another constraint is its mechanical strength though it is mallea111121`ble and sturdy, Shrilk, in comparison to widely used polymers such as polypropylene or polystyrene, exhibits limitations in terms of durability. This limitation hinders its application in scenarios requiring high strength or prolonged durability. To overcome these performance constraints, researchers and manufacturers are actively exploring methods of enhancing Shrilk's characteristics. Material modification and innovative processing techniques are being investigated to surpass these limitations. Potential strategies include increasing Shrilk's mechanical strength by modifying the chitin-to-silk ratio in the fabric or incorporating reinforcing fibers. Additionally, the material's resistance to chemicals and moisture could be bolstered by introducing coatings or additives. These approaches signify ongoing efforts to advance Shrilk's performance attributes. Considering all the parameters of suture material, properties of shrilk we came across while studying about the biomaterial shrilk, we suggest that shrilk can replace currently used suture materials with less complications and we also suggest that further research is required in this field.
6. CONCLUSION
The biomaterial Shrilk, a fusion of chitosan and fibroin derived from shrimp shells and silk, stands out as a promising candidate for sutures in surgical applications. The unique combination of properties, including exceptional strength, biocompatibility, biodegradability, and antimicrobial qualities, positions Shrilk as a potential alternative to traditional synthetic sutures. Its origin from natural sources reduces the likelihood of adverse reactions and tissue irritation, contributing to improved patient comfort during the healing process.
Comparative analysis with commonly used suture materials reveals that Shrilk exhibits superior tensile strength and breaking strain, crucial for effective wound closure. While challenges such as sensitivity to moisture and potential hydrolysis exist, these limitations could be addressed through material modification and processing methods. The incorporation of cross-linking agents or additives may enhance stability and toughness, while research into new processing methods could further improve mechanical strength and durability. The versatility of Shrilk allows for customization of its degradation rate, transparency, and bioadhesive properties, offering a tailored approach for diverse surgical needs. However, it is important to acknowledge that Shrilk's clinical use requires rigorous testing, regulatory approvals, and further research to fully understand its potential applications and address existing challenges. Despite its current limitations, Shrilk presents a novel and environmentally friendly biomaterial with the potential to revolutionize the field of surgical sutures.
In conclusion, while Shrilk shows great promise as a biomaterial for sutures, ongoing research is necessary to optimize its performance, overcome existing challenges, and ensure its safety and efficacy in diverse clinical settings. The journey towards the widespread adoption of Shrilk in medical practice requires collaborative efforts from researchers, clinicians, and regulatory bodies to unlock its full potential and contribute to advancements in surgical materials.
CONFLICT OF INTERESTS
None.
ACKNOWLEDGMENTS
We sincerely thank Vidyalankar Institute of Technology for providing resources towards this paper, we are extremely grateful towards Dr. Vidya Chitre, Professor, Information Technology, VIT for her invaluable guidance and support throughout the paper.
REFERENCES
Al Qattan, M. M., & KFoury, H. (2015). A Delayed Allergic Reaction to Polypropylene Suture used in Flexor Tendon Repair. The Journal of Hand Surgery, 40(7), 1377-1381. https://doi.org/10.1016/j.jhsa.2015.03.004
Bibire, T. Yilmaz, O., Ghiciuc, C.M., Bibire, N., & Dănilă, R. (2022). Biopolymers for Surgical Applications. Coatings, 12(2), 211. https://doi.org/10.3390/coatings12020211
Byrne, M. (2019). The Surgical Suture. Aesthetic Surgery Journal, 39(S2), S67-S72. https://doi.org/10.1093/asj/sjz036
Camlibel, N. O. (2004). Usage of Biopolymers in Medical Applications, Conference: 3rd Indo-czech Textile Research Conference.
Camlibel, N. O., & Sariisik, M. (2004). Using and Properties Biofibers Based on Chitin and Chitosan on Medical Applications. Conference: 3rd Indo-czech Textile Research Conference.
Chu, C.C. (1981). Mechanical Properties of Suture Materials: An Important Characterization. Annals of Surgery, 193(3), 365-371. https://doi.org/10.1097/00000658-198103000-00021
Dart, A.J., & Dart, C.M. (2011). Suture Material : Conventional and Stimuli Responsive. Comprehensive Biomaterials, 6. https://doi.org/10.1016/B978-0-08-055294-1.00245-2
Faris, A., & Khalid, L. (2022). Characteristics of Suture Materials Used in Oral Surgery: Systematic Review. International Dental Journal, 72(3), 278-287. https://doi.org/10.1016/j.identj.2022.02.005
Fernandez, J.G., & Ingber, D.E. (2012). Unexpected Strength and Toughness in Chitosan-Fibroin Laminates Inspired by Insect Cuticle. Adv. Mater., 24, 480-484. https://doi.org/10.1002/adma.201104051
Goel, A. (2016). Surgical Suture- A Review. Delhi Journal of Opthamology, 26(3), (159-162). https://doi.org/10.7869/djo.161
Harvard University (2011, December 13). Shrilk: Inspired by Insect Cuticle, a Low-Cost Material.
Meril Life Sciences Pvt. Ltd. (n.d.). Types of Surgical Sutures and Their Uses. Meril Life Sciences.
Meyle, J. (2006). Suture Materials and Suture Techniques. Perio, 3(4), 253-268.
Naleway, S. E., Lear, W., Kruzic, J. J., & Maughan, C. B. (2015). Mechanical Properties of Suture Materials in General and Cutaneous Surgery. Journal of Biomedical Materials Research, Part B, Applied Biomaterials, 103(4). https://doi.org/10.1002/jbm.b.33171
Thomas, S., Coates, P., Whiteside, B., Joseph, B., & Nair, K. (2003). Advanced Technologies and Polymer Materials for Surgical Sutures. Woodhead Publishing.
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© Granthaalayah 2014-2024. All Rights Reserved.