
UNILATERAL PULMONARY ARTERY ATRESIA/AGENESIS: A CASE REPORT
Olvis Petre 1![]()
![]() ,
Tashi Bani Irma 1,
Hasani Jola 1,
Shestani Justi 1, Bala Silvana 1, Hafizi Hasan 1
,
Tashi Bani Irma 1,
Hasani Jola 1,
Shestani Justi 1, Bala Silvana 1, Hafizi Hasan 1
1 Pulmonology Department, “Shefqet Ndroqi” University
Hospital, Albania
|
|
ABSTRACT |
||
|
A twenty-three-year-old male truck driver with a 12-pack year smoking history and no previous history of hospitalization was admitted to the “Shefqet Ndroqi” University Hospital pulmonology department after a cardiologist consultation where he was diagnosed with pulmonary hypertension. Two of the patient’s uncles from his mother’s side died during their pediatric age from congenital heart defects. A contrast-enhanced chest computed tomography was performed, and it showed an interruption of the lumen of the proximal part of the left pulmonary artery (atresia), a reduction of the left lung parenchyma volume, and bilateral pulmonary emphysema. The respiratory functional tests detected a moderate obstructive syndrome, and the 6MWT detected a decrease in arterial partial pressure of oxygen and oxygen saturation level. A diagnosis of unilateral pulmonary artery atresia/agenesis was confirmed. |
|||
|
Received 03 November 2022 Accepted 05 December 2022 Published 31 December 2022 Corresponding Author Olvis Petre, olvispetre@yahoo.com
DOI10.29121/granthaalayah.v10.i12.2022.4930 Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2022 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
Keywords: Unilateral Pulmonary Artery
Atresia/Agenesis, Pulmonary Hypertension, Isolated Pulmonary Artery Agenesis |
|||
1. INTRODUCTION
Embryological development aberration in the primary pulmonary vasculature may result in the absence of either one of the pulmonary arteries. Truncus arteriosus, pulmonary atresia, atrial septal defect, tetralogy of Fallot, and coarctation of the aorta are some of the additional congenital cardiovascular defects that are frequently linked to unilateral pulmonary artery atresia/agenesis (UPAA). Cucci et al. (1964).
Early childhood and the newborn stage are typically the times when developmental lung abnormalities are discovered. In the adult patient, the diagnosis of UPAA is most commonly incidental. Frentzel was the first to report the unilateral absence of the pulmonary artery. Fraentzel (1868) The solitary unilateral absence of the pulmonary artery is brought on by an aberrant sixth branch arch morphology. It is a rare disorder. There are about 200,000 to 300,000 adults are with isolated UPAA lacking other cardiac malformations. Kruzliak et al. (2013)
Chest radiographs may help, although a computed tomography is necessary to confirm the diagnosis. Due to its combination of several technological advancements, multidetector CT is the best noninvasive method for determining congenital lung defects such as UPAA. Lee et al. (2008)
In UPAA, right-sided engagement outnumbers left-sided involvement in frequency. Both the afflicted lung and the hilum are reduced in size. Zylak et al. (2002)
Many adults with UPAA frequently experience unusual symptoms such as exertional dyspnea, hemoptysis, and recurring infections. The presence of exertional dyspnea should prompt an investigation into the evaluation of pulmonary hypertension. Radiologically speaking, pulmonary parenchyma can be affected too. CT scans show abnormalities such as emphysema (often compensatory), bronchiectasis, and interstitial changes. Wang et al. (2017)
2. CASE REPORT
Our patient was admitted to the “Shefqet Ndroqi” University Hospital pulmonology department with a history of exertional dyspnea, extreme fatigue, and occasional smoking-related hemoptysis episodes during the last year. Ten days prior to the admission, he suffered from a lipothymia attack and had a chest X-ray performed. The chest X-ray revealed an increased cardiothoracic ratio, for which he was referred to a cardiologist.
The cardiologist performed a trans-esophageal echocardiography (TEE) which described an asynchrony of the interventricular septal movement, a mild mitral regurgitation, hypertrophy, and dilatation of the right ventricle (45 mm), dilatation of the right atrium (55 mm), moderate tricuspidal regurgitationdete, and an increased PASP of 55 mmHg. The interatrial and interventricular septae were intact. The bubble test was negative for a right-to-left shunt in basal conditions and after the Valsalva maneuver. He was then referred to a pulmonology consultation for further investigation.
The patient was a twenty-three-year-old male truck driver with a 12-pack year smoking history and no previous history of hospitalization or serious illnesses. He recalls being told by his mother that two of his uncles from his mother’s side died during their pediatric age from congenital heart defects.
On auscultation, an enhancement of the second cardiac tone could be detected. The rest of the patient's physical examination and laboratory examinations were unremarkable.
A forced spirometry evaluation was performed on the day of the hospitalization, and it showed a moderate to severe obstructive syndrome (FVC = 73.8%; FEV1 = 50.8%; FEV1/FVC = 55.77; PEF = 63.1%).
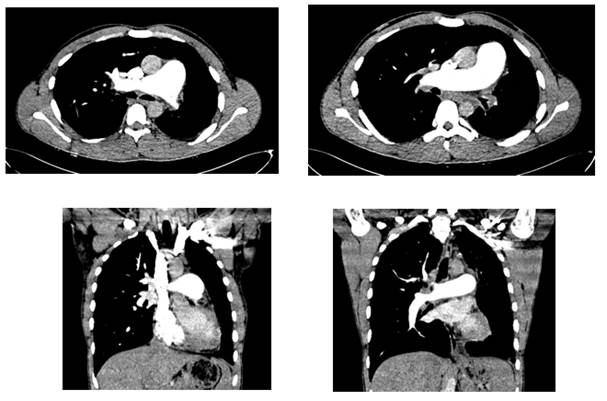
A contrast-enhanced chest computed tomography was performed, and it showed a mediastinal shift toward the left, an interruption of the lumen of the proximal part of the left pulmonary artery (atresia), with peripheral collateral vasculature. Figure 1
Figure 1
|
Figure 1 Axial and Coronal View from the Contrast-Enhanced CT Showing the Left Pulmonary Artery’s Lumen Interruption |
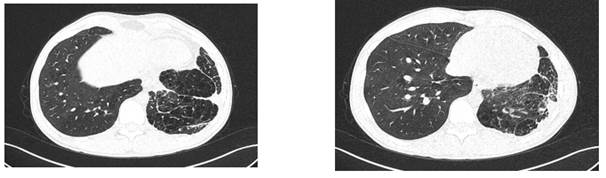
The CT also showed a reduction of the left lung parenchyma volume, which presented emphysematous (with multiple and confluent emphysemas in the lower fields due to oligaemia). Emphysemas were detected even in the right lung, which presented with an increased volume. Pleuro-parenchymal adherences, sub-pleural fibrotic reticular thickening, and a minimal left pleural effusion were also detected. Figure 2 A prominent right pulmonary artery (34 mm) with a compensatory dilatation of all the right vasculature was detected.
Figure 2
|
Figure 2 Axial Scans of the Chest CT Showing Lung Parenchymal Involvement |
Before discharge, another respiratory functional test (body plethysmography) confirmed the presence of a moderate obstructive syndrome. (FVC = 82.4%; FEV1 = 63.9%; FEV1/FVC = 62.75; PEF = 75.1%; TLC = 114.6% (7.91 L))
The Six-Minute Walk Test (6MWT) showed a decline of 10 mmHg in the partial pressure of oxygen on arterial blood gasses (66.5 mmHg vs. 56.5 mmHg) and a decrease in the level of oxygen saturation of 3.5 % (93.9% vs. 90.4%)
It was concluded that the patient suffered from Left Unilateral Pulmonary Artery Atresia/Agenesis (UPAA) with secondary pulmonary hypertension, COPD group D with pulmonary emphysema, and Acute on Chronic respiratory failure.
3. DISCUSSIONS
As of November 2022, there are 60 papers published on PubMed with the title "Unilateral pulmonary artery agenesis," but actual prevalence remains challenging to establish. The results of the physical examination are typically normal, with the exception of diminished breath sounds on the side that was affected. The ECG and arterial blood gas values are also normal.
Early diagnosis aids in the condition's management as it reduces the effects of recurrent infections on the pulmonary parenchyma. From what is known in the literature, there is no predilection for the right or the left side. There is, however, a more significant number of case reports linking right pulmonary agenesis with concomitant cardiac abnormalities. Therefore, left pulmonary artery agenesis is associated with fewer life-threatening complications. Zylak et al. (2002)
There is no universal agreement regarding UPAA treatment in adults. Wang et al. (2017) For patients who show no signs of cardiopulmonary impairment, no therapy is necessary. Most adults with UPAA are closely observed for an extended period. Shakibi et al. (1978)
Since the patent ductus arteriosus regresses throughout the first year of life, early surgical repair of UPAA in pediatric patients is preferable. Afterward, many arterial hypoplastic alterations restrict the surgical options. Surgery may be considered in some adult cases when persistent bleeding might reduce the patient's quality of life. Apostolopoulou et al. (2002)
4. CONCLUSIONS
Unexplained hemoptysis or exertional dyspnea should always prompt suspicion of pulmonary vasculature anomalies, such as UPAA. Early diagnosis and management are essential for the avoidance of life-threatening complications. However, there is no consensus in terms of treatment appropriateness. A multidisciplinary team should closely observe asymptomatic adult patients with UPAA constituted of pulmonologists, cardiologists, cardiac surgeons, vascular surgeons, and radiologists for adequate follow-up and management approach.
CONFLICT OF INTERESTS
None.
ACKNOWLEDGMENTS
None.
REFERENCES
Apostolopoulou, S. C., Kelekis, N. L., Brountzos, E. N.,
Rammos, S., And Kelekis, D. A. (2002). ‘Absent’ Pulmonary Artery in One
Adult and Five Pediatric Patients: Imaging, Embryology, And Therapeutic
Implications. AJR. American Journal of Roentgenology, 179(5), 1253–1260. https://doi.org/10.2214/ajr.179.5.1791253.
Cucci, C. E., Doyle, E. F., and Lewis, Jr., E. W. (1964). Absence of a Primary Division of the Pulmonary Trunk: An Ontogenetic Theory. Circulation, 29(1), 124–131. https://doi.org/10.1161/01.cir.29.1.124.
Fraentzel,
O. (1868). Ein Fall Von Abnormer Communication Der Aorta Mit Der Arteria
Pulmonalis. Archiv Für Pathologische Anatomie Und Physiologie Und Für Klinische
Medicin, 43(3), 420–426.
https://doi.org/10.1007/BF01915623.
Kruzliak, P., Syamasundar, R. P., Novak, M., Pechanova, O., and Kovacova, G. (2013). Unilateral Absence of Pulmonary Artery: Pathophysiology, Symptoms, Diagnosis and Current Treatment. Archives of Cardiovascular Diseases, 106(8–9), 448–454. https://doi.org/10.1016/j.acvd.2013.05.004.
Lee, E. Y., Boiselle, P. M., and Cleveland, R. H. (2008). Multidetector CT Evaluation of Congenital Lung Anomalies. Radiology, 247(3), 632–648. https://doi.org/10.1148/radiol.2473062124.
Shakibi, J. G., Rastan, H., Nazarian, I., Paydar, M., Aryanpour, I., and Siassi, B. (1978). Isolated Unilateral Absence of the Pulmonary Artery Review of the World Literature and Guidelines for Surgical Repair. Japanese Heart Journal, 19(3), 439–451. https://doi.org/10.1536/ihj.19.439.
Wang, P., Yuan, L., Shi, J., and Xu, Z. (2017). Isolated Unilateral Absence of Pulmonary Artery in Adulthood: A Clinical Analysis of 65 Cases from a Case Series and Systematic Review. Journal of Thoracic Disease, 9(12), 4988–4996. https://doi.org/10.21037/jtd.2017.11.49.
Zylak, C. J., Eyler, W. R., Spizarny, D. L., and Stone, C. H. (2002). Developmental Lung Anomalies in the Adult: Radiologic-Pathologic Correlation. Radiographics, 22 Spec No (Suppl_1), S25–S43. https://doi.org/10.1148/radiographics.22.suppl_1.g02oc26s25.
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© Granthaalayah 2014-2022. All Rights Reserved.