
PREVALENCE OF CERVICOGENIC HEADACHE AMONG YOUNG POPULATION
Dr. Vadivelan Kanniappan 1![]()
![]() ,
Shalu Sam
Abraham 2
,
Shalu Sam
Abraham 2![]() , T. S. Veeragoudhaman 3
, T. S. Veeragoudhaman 3![]()
1 PhD.,
Professor, SRM College of Physiotherapy, SRM Institute of Science and
Technology, SRM Nagar, Kattankulathur – 603202, Kancheepuran, Tamilnadu, India
2 M.P.T.,
PhD. Professor, SRM College of Physiotherapy, SRM Institute of Science and
Technology, SRM Nagar, Kattankulathur – 603202, Kancheepuran, Tamilnadu, India
3 M.P.T.,
M.S.W. Dean, SRM College of Physiotherapy, SRM Institute of Science and
Technology, SRM Nagar, Kattankulathur - 603203.
Kancheepuram, Chennai, Tamilnadu India
|
|
ABSTRACT |
||
|
Background: Cervicogenic headache (CEH) is a secondary headache characterized by unilateral headache, signs of neck involvement and often worsened by neck movement, sustained awkward head position. Excessive stress to the neck, degenerative conditions like osteoarthritis, a prolapsed disc in the neck, or a whiplash injury can cause cervicogenic headache. The current young generation uses smart phones for a high amount of time. The researchers found that there is a strong positive correlation with pain intensity, headache and neck disability index suggested that long time use of Smartphone had a strong relationship with neck pain. The first line treatment for cervicogenic headache is physiotherapy management. Objective: To check the prevalence of cervicogenic headache among young population. Methodology: Nonexperimental and observational type. Outcome Measures: Prevalence of Cervicogenic Headache Questionnaire (Self prepared questionnaire). Procedure: Subjects were selected according to inclusion criteria; the questionnaires were sent and later it was scored, and statistics were made. Results: The study shows that there is prevalence of cervicogenic headache among young population. Among the 272 individuals 26 individuals showed proneness to cervicogenic headache. Conclusion: the study concludes that there is 10.4% prevalence and proneness of cervicogenic headache among young population, it can be due to the strain in the neck while using Smartphone, laptops or while doing other activities like studying, playing games. |
|||
|
Received 10 August 2022 Accepted 11 September 2022 Published 23 September 2022 Corresponding Author Dr. Vadivelan Kanniappan, vadivelk@srmist.edu.in DOI10.29121/granthaalayah.v10.i9.2022.4706 Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2022 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
Keywords: Cervicogenic Headache, Young Population,
Prevalence |
|||
1. INTRODUCTION
Cervicogenic headache involves single-sided headache with
manifestations and indications of the neck involvement. The cervicogenic
headache (CEH) is mostly diagnosed incorrectly or mistaken for other types of headaches.
The CEH diagnosis has been evolving over the years and is given by the
international headache society (IHS). The International Classification
of Headache Disorders (ICHD BETA 3) defined “Headache caused by a disorder
of the cervical spine and its component bony, disc and/or soft tissue elements,
usually but not invariably accompanied by neck pain is called cervicogenic
headache. Blumenfeld and Siavoshi (2018)
Criteria for the diagnosis of CEH were published by Sjaastad et al in 1990 with a revision in 1998. Van et al. (2003). Headache is classified by the international Headache society. The 3rd edition of international classification of headache disorders (ICHD) is an in-depth classification of headaches containing diagnostic criteria for headache disorders. They have classified headaches into Primary, secondary, painful cranial neuropathies, and other facial pain. Primary headache includes migraine, tension type headache etc which is not caused by underlying disease or any structural problems. The secondary headaches are hypothesized to be symptoms of an underlying disease or structural problems Cephalalgia (2018). Hence cervicogenic headache is an example of a secondary headache because in this case the main disorder is dysfunction within the cervical structures which is upper cervical segments Bogduk and Govind (2009).
The cause of cervicogenic is hypothesized because of the structural problems of C2 and C3 and also for people who has work / job related to straining neck for example drivers, hairstylists, carpenters these jobs are more likely to develop cervicogenic headache.
The pain which causes the cervicogenic headache is hypothesized as the cervical structures and its attachment to the bone and capsule of the intervertebral joints and discs, ligaments, nerve, and nerve roots. In muscle trapezius when the electromyographic activity was recorded it portrayed higher in the symptomatic side than on the asymptomatic side, but this just a hypothesis and it is not a confirmed study that symptomatic side shows more electro-myographic activity than the asymptomatic side. Only in cervicogenic headache group noticeable irregularity in skin-fold tenderness was found and side difference was limited to the trapezius region.
One of study based on prevalence of cervicogenic headache among general population aged 20-59 done in demark in 1993 showed that there were 14% to 16% patients fulfilled cervicogenic headache criteria and this study used the old version of diagnostic criteria which is 1990 criteria of the international headache society for diagnosing cervicogenic headache. A recent article from the year 2009 showed that there is prevalence of cervicogenic headache has been estimated to be 4.1% in general population and as high as 17.5% among patients with severe headache.
And another study was conducted among university students who use Smartphone’s and was divided according to the usage of phone. The results turned out to be there is prevalence of headache among students who use more Smartphone’s but what type of headache was not identified. Demirci et al. (2016) Kim et al. stated that prolonged use of Smartphone will lead to postural changes in lumbar and cervical vertebrae and also proprioception deficits in the cervical vertebrae.
Initially the diagnosis of cervicogenic headache was done in 1990 and later altered in the year 1998. The latest panel of clinical criteria includes seven criteria for the diagnosis. Articles stated that if the pain started or originated in neck before the headache, if the headache is unilateral, provocation of pain due to neck movement are the main dependable features for diagnosis of cervicogenic headache. But no studies have confirmed that patients who satisfied these diagnostic criteria actually have a cervical source for their pain.
Many studies and systematic reviews have been done based on cervicogenic headache treatment stating that physiotherapy is the first line of treatment. Jull et al. (2002) People who experience neck pain commonly are seen to experience more headaches than the people who don’t experience it. It can be due to the strain given in the cervical region.
2. AIM OF THE STUDY
To
study the prevalence of cervicogenic headache among young population
3. NEED OF THE STUDY
Cervicogenic headache is often misdiagnosed and treated inadequately because of confusing and varying terminology and is usually mistaken as other primary headache such as tension type headache and migraine. There are no studies done based on the prevalence of cervicogenic headache in South India.
There is increasing literature on the diagnosis and treatment of CEH, but epidemiological data are scarce. There are studies done among students which show students who use Smartphone’s for high amount of time experience frequent headaches, it can be due to cervical related problems or other type of headaches.
4. METHODOLOGY
STUDY DESIGN : Non-experimental
STUDY TYPE : Observational Type
SAMPLING METHOD : Convenient Sampling Method
SAMPLING SIZE : 272
STUDY SETTING : Online Google form
5. INCLUSION CRITERIA
Young population aged 15-24 years.
Both men and women included.
Subjects who experience frequent headaches.
Subjects who spend excess amount of time using computers/laptops/phones.
6. EXCLUSION CRITERIA
Recent fractures.
Individuals
who are not willing to participate
Recent surgeries.
Congenital conditions of cervical spine.
7. PROCEDURE
IEC 2229/IEC/2020 was obtained before starting the study. A set of 15 questions were made initially based on the diagnosis of cervicogenic headache. Initially a small pilot study was done among 20 students with the 15 set of questions, they were aged 18-21 and the sensitivity, specificity of the questionnaire was checked. Sensitivity was 0.5% and specificity was 0.8%. The questionnaire was then sent to physiotherapists who specialized in cervicogenic headache for validation. It was then validated and one more question was added which finally made to 16 set of questions. The questionnaire was then sent to individuals aged 15-24 through Google forms as the present pandemic situation, it was the only way possible. The subjects were selected according to inclusion criteria. The questionnaires were filled but few of the forms had to be omitted due to age criteria as those were above the age of 24 years, the final forms were 272 in number. The forms were then scored, and statistical analysis was done. The set of 16 questions were as follows.
1) Do you have frequent headaches?
2) How many days during the last 2 months have you had headache?
3) How long does your headache last?
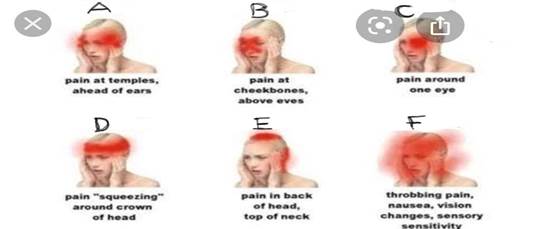
4) Choose the option where the headache is confined to mostly (side)
5) Mention
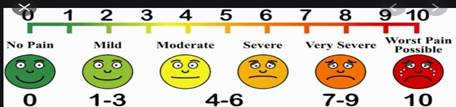
according to scale how intense is the pain
6) How
many hours do you spend sitting in front of laptop/computer in a day?
7) What
neck posture do you use your phone?

8) Do
you have neck pain prior to your headache? Yes/No
9) Is
your headache unilateral (one sided)
10) Does the
pain get triggered by neck movement or external pressure at back of the neck or
awkward posture? Yes/No
11) Does your
headache hinder your daily activity? Yes/No
12) Do you
have any other symptom along with headache? if yes please do mention.
13) Is sound
bothersome when you experience headache? Yes/No/Sometimes
14) Does water
come out of your eyes automatically during headache? Yes/No
15) Do you
feel any kind of dizziness during the headache? Yes/No/Sometimes
16) If yes for
dizziness (above question), then select the below option for what kind of
dizziness.
· Vague sensation of floating
· Spinning like the whole room is spinning
· Sensation of unsteadiness
8. SCORING
1) Yes – 1
No – 0
2) (A) – 1
(B) – 2
(C) - 3
(D) – 4
3) Open ended question
4) (A)– 1
(B) – 2
(D) – 3
(C) – 4
(D) – 5
(E) – 6
5) As per pain scale
6) (A) Less than 2 hours – 1
(B) 2-4 hours – 2
(C) 4-6 hours – 3
(D) 6-8 hours – 4
(E) 8-10 hours – 5
(F) more than 10 hours – 6
7) (A)– 1
(B) – 2
(C) – 3
(D) – 4
(E) – 5
8) (A) Yes – 1
(B) No – 0
9) (A) Yes – 1
(B) No – 0
10) (A) Yes – 1
(B) No – 0
11) (A) Yes – 1
(B) No – 0
12) (A) Yes – 2
(B) No – 0
(C) Sometimes – 1
13) No score
14) (A) Yes – 0
(B) No – 1
15) (A) Yes – 2
(B) No – 0
(C) Sometimes – 1
16) (A)– 1
(B) – 2
(C) – 3
MINIMUM SCORE – 5
MAXIMUM SCORE – 34
9. DATA ANALYSIS
The data collected was analysed using IBM Social Statistical System (SPSS) version 2.0 for windows that were used for data analysis.
Table 1
|
Table 1 Proneness to Cervicogenic Headache |
|||||||
|
Count of Age |
Score |
22 |
23 |
24 |
25 |
26 |
Grand Total |
|
16 |
|
|
2 |
|
|
|
2 |
|
17 |
|
1 |
|
|
1 |
|
2 |
|
19 |
|
|
2 |
|
1 |
1 |
4 |
|
20 |
|
2 |
1 |
2 |
|
1 |
6 |
|
21 |
|
1 |
3 |
|
1 |
|
5 |
|
22 |
|
1 |
1 |
|
1 |
|
3 |
|
23 |
|
|
2 |
|
1 |
|
3 |
|
24 |
|
|
1 |
|
|
|
1 |
|
Grand total |
|
5 |
12 |
2 |
5 |
2 |
26 |
According to Table 1 there are total of 26 individuals who are above the score of 22 and above which is proneness to cervicogenic headache.
10. BAR DIAGRAM I
PRONENESS TO CERVICOGENIC HEADACHE
Chart 1
|
|
|
Chart 1 Shows
Individuals who Got a Score of 22 and Above which Shows Proneness to
Cervicogenic Headache |
Table 2
|
Table 2 Gender - Female |
|
|
Row labels |
Count of gender |
|
6 |
1 |
|
7 |
8 |
|
8 |
5 |
|
9 |
4 |
|
10 |
10 |
|
11 |
15 |
|
12 |
13 |
|
13 |
18 |
|
14 |
15 |
|
15 |
11 |
|
16 |
4 |
|
17 |
12 |
|
18 |
14 |
|
19 |
12 |
|
20 |
11 |
|
21 |
3 |
|
22 |
3 |
|
23 |
10 |
|
24 |
2 |
|
25 |
4 |
|
26 |
1 |
|
Grand total |
176 |
Table 2 shows the total number of female responses with the scores, there is a total of 176 female responses.
11. BAR DIAGRAM II
GENDER- FEMALE
Chart 2
|
|
|
Chart 2 Shows the Number of
Female Responses with the Scores. |
Table 3
|
Table 3 Gender- Female |
|
|
Row labels |
Count of gender |
|
6 |
1 |
|
7 |
8 |
|
8 |
5 |
|
9 |
4 |
|
10 |
10 |
|
11 |
15 |
|
12 |
13 |
|
13 |
18 |
|
14 |
15 |
|
15 |
11 |
|
16 |
4 |
|
17 |
12 |
|
18 |
14 |
|
19 |
12 |
|
20 |
11 |
|
21 |
3 |
|
22 |
3 |
|
23 |
10 |
|
24 |
2 |
|
25 |
4 |
|
26 |
1 |
|
Grand total |
176 |
Table 3 shows the total number of male responses with the scores, there is a total of 96 responses.
12. BAR DIAGRAM III
GENDER- MALE
Chart 3
|
|
|
Chart 3 Shows
Number of Male Responses with the Scores, there is a Total of 96 Male
Responses |
Table 4
|
Table 4 Area Where the Headache is Confined |
|||||||||||
|
Row labels |
15 |
16 |
17 |
18 |
19 |
20 |
21 |
22 |
23 |
24 |
Grand total |
|
A |
2 |
2 |
4 |
12 |
14 |
15 |
32 |
15 |
5 |
2 |
103 |
|
B |
|
|
2 |
3 |
2 |
1 |
10 |
3 |
1 |
|
22 |
|
C |
|
|
1 |
4 |
|
6 |
6 |
4 |
2 |
|
23 |
|
D |
|
4 |
9 |
11 |
6 |
9 |
24 |
8 |
6 |
3 |
80 |
|
E |
|
|
2 |
4 |
6 |
5 |
6 |
4 |
1 |
1 |
29 |
|
F |
|
|
|
1 |
2 |
4 |
4 |
2 |
2 |
|
15 |
|
Grand total |
|
2 |
6 |
18 |
35 |
30 |
40 |
82 |
17 |
6 |
272 |
Table 4 shows the area where the headache is confined to, A, B, C, D, E, F are the options with the Age group and the respective number of responses.
13. BAR DIAGRAM IV
AREA WHERE THE HEADACHE IS CONFINED
Chart 4
|
|
|
Chart 4 Represents the Area of Where the
Headache is Confined to, A, B, C, D, E, F are the Options with the Age Group and
the Respective Number of Responses |
14. RESULTS
Based on bar chart 1, it shows the number of people above the score of 22 and the age. The Y axis is number of people having the specific score, the X axis shows the age of people, and the bar depicts the score from 22 and above. The scoring is from 5 which is the minimum score to 34 which is the maximum score. There is a total of 26 subjects whose score is 22 and above which depicts proneness to cervicogenic headache.
Based on bar chart 2, it’s the gender chart showing the score. In chart 2 it’s the female scoring. The X axis shows the number of people having the specific score and the Y axis shows the score from 6 to 26. Out of 272 responses 176 responses are of females and out of those 20 females had a score of 22 and above which is proneness to cervicogenic headache. Compared to males, female responses were more in count.
Based on bar chart 3, it’s also the gender chart showing the score. In this chart it shows the male scoring. The X axis shows the number of people having the specific score and the Y axis shows the score from 6 to 26. Out of 272 responses 96 were male responses. In the 96 responses 6 of the responses were having score 22 and above.
Based on bar chart 4, it shows the area of headache where it is confined to and how many people fall into each category. The X axis shows each option from A to F which people chose, and the Y axis shows the number people who chose the specific option. The right side of the chart shows the age of subjects with different colours which is the bar in the chart. Option A shows more prevalence which is 103 and age group 21 is more in this, followed by option D (80 individuals), option E (29), option C (23), option B (22), option F with the least number of individuals which is 15.
15. DISCUSSION
Aim of the study is to find the prevalence of cervicogenic headache among young population and this study shows that there is prevalence of cervicogenic headache among young population.
A total of 272 subjects were taken and in those 26 subjects showed proneness to cervicogenic headache which is 10.4% of the samples. Among the 276 responses 176 responses were female and 96 were male. Out of 276 responses 91 responses stated ‘Yes’ to having frequent headaches. The questionnaire consisted of 16 questions with a minimum score of 5 and maximum score of 34. A score from 22 and above is the indication of cervicogenic headache. In this study the questionnaire was formed or made based on the diagnosis criteria of cervicogenic headache.
The diagnosis of cervicogenic headache remains controversial but there are studies done showing validity to the clinical diagnosis. The epidemiological data is scarce but there is increased literature for the treatment, quality of life and diagnosis of the headache. Cervicogenic headache is secondary type of headache which many people are not aware of and is often mistaken for other types of headaches, so it is important to diagnose correctly and give proper treatment.
The exact cause of cervicogenic headache is unknown but it is hypothesized as cervical origin which can be due to strain. The prolonged use of Smartphone’s, laptops might be a reason as in the questionnaire most of them has chosen option for the posture of using Smartphone in an extreme flexed position of neck. In a study done by Demirci et al. (2016) suggested that headache maybe associated with Smartphone use. But they haven’t mentioned what type of headache it is.
A study done by Nilsson (1995) among general population using a questionnaire concluded that cervicogenic headache is a common form of headache, similar to migraine in prevalence. But in younger population, the prevalence study is scarce, so this study has helped to identify even the younger population is prone to cervicogenic headache.
It is important to identify people who are experiencing cervicogenic headache and give them the right treatment. A study done by Van et al. (2003), about quality of life of patients with cervicogenic headache showed that patients had domain scores for physical functioning and have a quality-of-life burden that is substantial. Physiotherapy treatment is the first line of treatment for cervicogenic headache.
A study done by Chaibi and Russell (2012) about manual therapies for cervicogenic headache: a systematic review, they concluded that the randomized controlled trail suggests that physiotherapy might be an effective treatment in the management of cervicogenic headache. So, it is important to identify the signs or proneness to headache so the proper treatment can be given.
16. CONCLUSION
The study concludes that there is prevalence and proneness of cervicogenic headache among young population, it can be due to the strain given to cervical region by using phone or laptop in flexed position or it can be even due to studying with the neck in flexed position for a long time. With the help of strengthening exercises (including deep neck flexors) and cervical rotation (self-mobilization) the cervicogenic headache can be prevented or managed. It is important to identify the type of headache and give the proper treatment at a early stage. Cervicogenic headache is secondary type of headache which many people are not aware of and is often mistaken for other types of headaches, so it is important to diagnose correctly and give proper treatment.
17. LIMITATIONS AND RECOMMENDATIONS
17.1. LIMITATIONS
· Due to the pandemic the questionnaires had to be sent through google forms.
· The age limit was 15-24
17.2. RECOMMENDATIONS
· The sample size can be bigger
· Male participants could be more
· Detailed clinical diagnosis can be done.
CONFLICT OF INTERESTS
None.
ACKNOWLEDGMENTS
None.
REFERENCES
Beeton, K., and Jull, G. (1994). Effectiveness of Manipulative Physiotherapy in the Management of Cervicogenic Headache : A Single Case Study. Physiotherapy, 80(7), 417-23. https://doi.org/10.1016/S0031-9406(10)60788-2.
Blumenfeld, A., and Siavoshi, S. (2018). The Challenges of Cervicogenic Headache. Current Pain and Headache Reports, 22(7), 47. https://doi.org/10.1007/s11916-018-0699-z.
Bogduk, N. (1992). The Anatomical Basis for Cervicogenic Headache. Journal of Manipulative and Physiological Therapeutics, 15(1), 67-70.
Bogduk, N., and Govind, J. (2009). Cervicogenic Headache : An Assessment of the Evidence on Clinical Diagnosis, Invasive Tests, and Treatment. Lancet Neurol, 8, 959-68. https://doi.org/10.1016/S1474-4422(09)70209-1.
Cephalalgia (2018). Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd Ed. International Headache Society, 38, 1-211. https://doi.org/10.1177/0333102417738202.
Chaibi, A., and Russell, M.B. (2012). Manual Therapies for Cervicogenic Headache : A Systematic Review. The Journal of Headache and Pain, 13(5), 351-9. https://doi.org/10.1007/s10194-012-0436-7.
Demirci, S., Demirci, K., and Akgonul, M. (2016). Headache in Smartphone User : A Cross-Sectional Study. J. Neurol Psychol, 4(1), 5. https://doi.org/10.13188/2332-3469.1000025.
Haldeman, S., and Dagenais, S. (2001). Cervicogenic Headaches : A Critical Review. The Spine Journal, 1(1), 31-46. https://doi.org/10.1016/S1529-9430(01)00024-9.
Jull, G., Trott, P., Potter, H., Zito, G., Niere, K., Shirley, D., Emberson, J., Marschner, I., and Richardson, C. (2002). A Randomized Controlled Trial of Exercise and Manipulative Therapy for Cervicogenic Headache. Spine, 27(17), 1835-43. https://doi.org/10.1097/00007632-200209010-00004.
Knackstedt, H., Bansevicius, D., Aaseth, K., Grande, R.B., Lundqvist, C., and Russell, M.B. (2010). Cervicogenic Headache in the General Population : The Akershus Study of Chronic Headache. Cephalalgia, 30(12),1468-76. https://doi.org/10.1177/0333102410368442.
Nilsson, N. (1995). The Prevalence of Cervicogenic Headache in A Random Population Sample of 20-59 Year Olds. Spine, 20(17), 1884-8. https://doi.org/10.1097/00007632-199509000-00008.
Ogince, M., Hall, T., Robinson, K., and Blackmore, A.M. (2007). The Diagnostic Validity of the Cervical Flexion-Rotation Test in C1/2-Related Cervicogenic Headache. Manual Therapy, 12(3), 256-62. https://doi.org/10.1016/j.math.2006.06.016.
Sjaastad, O., Fredriksen, T.A., and Pfaffenrath, V. (1998). Cervicogenic Headache : Diagnostic Criteria. Headache : The Journal of Head Ond Face Pain, 38(6), 442-5. https://doi.org/10.1046/j.1526-4610.1998.3806442.x.
Van Suijlekom, H.A., Lamé, I., Stomp-van Den Berg, S.G., Kessels, A.G, and Weber, W.E. (2003). Quality of Life of Patients with Cervicogenic Headache : A Comparison with Control Subjects and Patients with Migraine or Tension-Type Headache. Headache, 43(10), 1034-41. https://doi.org/10.1046/j.1526-4610.2003.03204.x.
Zito, G., Jull, G., Story, I. (2006). Clinical Tests of Musculoskeletal Dysfunction in the Diagnosis of Cervicogenic Headache. Manual Therapy,11(2),118-29. https://doi.org/10.1016/j.math.2005.04.007.
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© Granthaalayah 2014-2022. All Rights Reserved.