
SURGICAL MANAGEMENT OF PATIENTS
DIAGNOSED WITH MALIGNANT PHYLLODES Tumour OF THE BREAST IN THE NATIONAL ONCOLOGY INSTITUTE: DR. JUAN TANCA MARENGO
(SOLCA - GUAYAQUIL)
Dr. Freddy
Rueda Safady 1, Dr. Fernando
Miñán Arana 2, Dr. Francisco Xavier Hernández Manrique 3, Dr. Pablo Ulloa
Ochoa 4![]()
![]()
1 General Surgeon at the Hospital Monte Sinaí
of Guayaquil, Ecuador
2 Professor at the University of Specialties Espíritu
Santo, Ecuador
3 Professor of Medicine at the University of Guayaquil, Ecuador
4 Professor of Medicine at the University of Guayaquil, Ecuador
|
|
ABSTRACT |
||
|
The aim is to establish the real relationship of incidence of the Malignant phyllodes Tumor of Breast and its effective surgical approach in patients treated at the Oncological Institute of Guayaquil, the reference center of Ecuador. Objective: To establish the surgical management of Malignant phyllodes Tumors of Breast in the Oncological Institute of Ecuador SOLCA. Method: An analysis of the cases diagnosed and operated in the Oncological Institute of Guayaquil SOLCA in the period September 2009 to September 2019, based on a retrospective descriptive study to determine the surgical management of phyllodes tumors is performed. Results: Within the study period (9 years), 24 patients with Malignant phyllodes Tumor of Breast who met the admission criteria were analyzed. Two groups were established: 75% (n = 18) who left “alive” from the hospital and 25% “deceased” (n = 6). An analysis of the mortality adjusted to the surgical procedure was performed, where it can be observed that the radical mastectomy showed a survival of 82%, while the simple mastectomy and the lumpectomy, procedures chosen as the first option for the treatment of the malignant phyllodes tumor, presented a Survival less than 40%. Conclusions: The phyllodes malignant breast tumor has a low incidence among
malignant breast tumors. It seems that radical mastectomy of the breast is
the best option for patients with this type of cancer, and adjuvance does not improve patient survival. |
|||
|
Received 16 March 2022 Accepted 16 April 2022 Published 30 April 2022 Corresponding Author Dr. Pablo
Ulloa Ochoa, pulloa_88@hotmail.com DOI 10.29121/granthaalayah.v10.i4.2022.4494 Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2022 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
Keywords: Malignant Phyllodes Tumor, Surgical
Technique, Mastectomy, Lumpectomy, Lymph Node Sampling, Breast Biopsy |
|||
1. INTRODUCTION
Phyllodes Tumour of the Breast, was named for the first time by Johannes Müller in 1838, has some synonyms such as adenomatous myxoma, pseudosarcoma adenoma, cystosarcoma phyllodes among others. The World Health Organization decided to use the term "Phyllodes Tumour" to name this disease formally in 2003. The incidence of benign breast tumours is 35-64%, while malignant breast tumours comprise 25% of cases. Juan et al. (2007), Firdaus et al. (2017), Francisco et al. (2009), Wang et al. (2018).
Phyllodes tumour of the breast corresponds to 0.5% to 1.0% of all breast tumours and 2.5% of all fibroepithelial tumours. Population-based estimates indicate that the incidence of malignant phyllodes tumour is 2.1 cases per million women, with more frequency in white, Latino, and Asian women. Primary phyllodes tumour of the breast is a tumour that is made up of stroma and tissue of epithelial origin, which is why it is classified as part of biphasic breast tumours. Jiménez-López et al. (2013), Tan et al. (2012), Kamitani et al. (2014), Santos et al. (2007).
Within the surgical treatment of malignant phyllodes tumour of the breast, the decision to perform a simple total mastectomy versus a lumpectomy is not well defined, due to the natural behaviour of this tumour. The phyllodes tumour of the breast can have an invasive growth at the local level, some parameters are taken regarding this, such as the size of the tumour being less than 3 cm, that its total resection can be carried out and jointly that it can have at least a margin greater than 1 cm at the edges of the surgical piece, which has palpable axillary nodes with high suspicion of malignancy, are the parameters that influence the decision- making of the surgical treatment to be performed. Santos et al. (2007), Diego et al. (2016), Sun et al. (2019), Pornchai et al. (2019), Adesoye et al. (2016).
The evolution of these patients is determined by the timely treatment of these lesions, among the types of biopsy used is the FNA diagnosis that reaches 9% of cases found, there are also alternatives such as an excisional biopsy in which the problem is to remove the tumour leaving compromised margins, misinterpreting it as a fibroadenoma due to its size and appearance on breast ultrasound, unfortunately there can be different types of phyllodes tumour in the same surgical piece, which is why when having a surgical piece with compromised edges, there is an increase in their morbidity and mortality. Parfitt et al. (2004), Nomura et al. (2006), Karihtala et al. (2016), Spitaleri et al. (2013),Testori et al. (2015).
2. MATERIAL AND METHOD
Descriptive, retrospective, In the present study the population is made up of the patients of the Oncology Institute of Guayaquil SOLCA in the period from September 2009 to September 2019, who were diagnosed with Malignant phyllodes Tumour that corresponded to 20 cases, being our sample these patients.
3. RESULTS
Within the study period (9 years), 5,655 patients were obtained who presented Malignant Breast Tumour, among whom 24 patients were diagnosed with Malignant Phyllodes Breast Tumour, who met the admission criteria, resulting in an incidence of 0 ,45%. Two groups were established: patients who were discharged “alive” from the hospital 75% (n= 18) and those who were discharged “deceased” 25% (n= 6)
Table 1
|
Table 1 Distribution of Age,
Comorbidities and Menarche (n= 24) |
||||||
|
|
Deceased
n= 6 |
Standard
deviation |
% |
Alive n=18 |
Standard
deviation |
% |
|
Age years
(average) |
52 |
16.9 |
|
51.9 |
9.1 |
|
|
Comorbidity (Patients) |
2 |
|
33.3% |
11 |
|
61.1% |
|
Menarche
(years) |
11 |
1.6 |
|
12.8 |
1.3 |
|
|
Own Elaboration Rueda (2019) |
||||||
The average age of the patients with Malignant Breast Tumour in the two groups "Alive" and "Deceased" was around 52 years with no statistical differences, and in terms of menarche there were no significant differences in the 2 groups ("Alive" 11 years vs "deceased" 12.8 years). There were greater comorbidities in the group of "Living" 61.1% vs. "Deceased" 33.3%.
Table 2
|
Table 2 Distribution Table
According to Tumor Size and Its Mortality |
||||
|
Tumour Size (Patients) |
Deceased N=6 |
Percentage |
Alive N=18 |
Percentage |
|
< 5 cm |
1 |
16.6% |
1 |
5.5% |
|
5 a 10 cm |
1 |
16.6% |
10 |
55.5% |
|
> 10 cm |
4 |
66.6% |
7 |
38.8% |
|
Own Elaboration Rueda
(2019) |
||||
It was observed that in the group of deceased patients there was a higher mortality rate in patients with a tumour size greater than 10 cm with 66.6% (n=4) and in the group of "alive" patients the highest survival was in patients with tumour from 5 to 10 cm with 55.5% (n=10).
Table 3
|
Table 3 Distribution on
Surgical Procedures, Mortality and Survival |
||
|
Surgical Procedure |
Living |
Deceased |
|
Modified Radical Mastectomy (N=
11) |
82% |
18% |
|
Simple Total Mastectomy (N=5) |
40% |
60% |
|
Lumpectomy (N= 8) |
25% |
75% |
|
Own Elaboration Rueda
(2019) |
||
The patients underwent a type of surgical procedure, which was performed by the professionals of the Institute, it was not performed by a single professional, an institutional protocol was not followed.
This table identifies that the highest survival rate was in patients who underwent Modified Radical Mastectomy with 82%, while the highest mortality was lumpectomy with 75%.
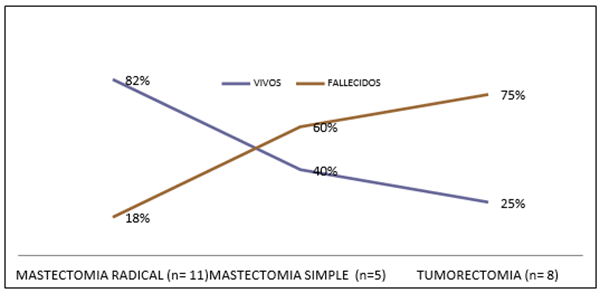
Graph 1
|
Graph 1 Mortality Adjusted to The Surgical Procedure Own Elaboration Rueda (2019) |
An analysis of the mortality adjusted to the surgical procedure was carried out, where it can be observed that the modified radical mastectomy presented a survival of 82%, while the total simple mastectomy and the lumpectomy, procedures chosen as the first option for the treatment of Malignant phyllodes Tumor, had a survival of less than 40%.
Table 4
|
Table 4 Patients Reoperated Due
to Presenting Edge Involvement by Malignant Philodes
Tumour of The Breast |
||||
|
Patients |
Living |
|
Deceased |
|
|
Compromised Edges |
6 |
33.30% |
5 |
83.30% |
|
Reoperated |
5 |
83% |
1 |
20% |
|
Own Elaboration Rueda
(2019) |
||||
In the Study, after the patients were operated on, the Pathological Anatomy Department reported the surgical piece with free edges due to the phyllodes tumour of the breast or as a surgical piece with edges compromised by the phyllodes tumour of the breast, in this table the patients are taken reoperated due to presenting borders compromised by the Malignant Phyllodes Tumour of the Breast.
It was observed in the sample of living patients with margins compromised by the phyllodes tumour of the breast (n=6), 5 patients were reoperated (83%) who obtained a higher survival than the deceased patients with 1 reoperated patient (20%) and 5 patients who were given adjuvant.
Table 5
|
Table 5 Surgically Intervened
Patients Who Received Adjuvance |
||||
|
Patients (N=24) |
Deceased (N=6) |
Percentage |
Alive (N=18) |
Percentage |
|
Adjuvanted |
4 |
66.6% |
8 |
44.4% |
|
Own Elaboration Rueda
(2019) |
||||
It can be seen that the patients who received adjuvant therapy (radiotherapy or chemotherapy), in deceased patients it was given in 4 patients with a percentage of 66.6% and in 8 living patients with a percentage of 44.4% respectively. The adjuvant therapy that was performed the most was radiotherapy; in deceased patients it was given in 4 patients with a percentage of 66.6% and in living patients it was in 6 patients with a percentage of 33.3%. It seems that adjuvant treatment occurred more in deceased patients, not obtaining an apparent benefit in the survival of patients with Malignant Phyllodes Tumour of the Breast.
4. DISCUSSION AND RECOMMENDATIONS
Malignant phyllodes tumour of the breast has a low incidence among malignant breast tumours. It seems that radical breast mastectomy is the best option for patients with this type of cancer, and adjuvant surgery does not improve patient survival. Lumpectomy was the surgical procedure that caused the most mortality.
References
Adesoye T, Neuman H.B et al. (2016). Current Trends in the Management of Phyllodes Tumors of the Breast, Annals of Surgical Oncology, 3199 – 3205. https://doi.org/10.1245/s10434-016-5314-0
Diego, D. et al. (2016). Phyllodes Tumor. State of the Art, Colombian Journal of Cancerology, 20(2), 79-86. https://doi.org/10.1016/j.rccan.2015.10.001
Firdaus, H. et al. (2017) Approaches to Phyllodes Tumours of the breast : a review article, International Surgery Journal, 4 (3),841-845. https://doi.org/10.18203/2349-2902.isj20170841
Francisco, T. G. et al. (2009). Tumor Filodes Maligno (Cystosarcoma filodes) mamario con diferenciación lipoblàstica. Estudio radiológico e histológico, Revista Española de Patología, 42 (3), 230-234. https://doi.org/10.1016/S1699-8855(09)70188-6
Jiménez-López, J. et al. (2013). Tumor Phyllodes, Perinatología y Reproducción Humana, 27 (2), 106-112. http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S0187-53372013000200006
Juan A. Pérez et al. (2007). Tumor Filodes du mama. Características clínica e Histopatológica de 39 casos, Revista chilena de cirugía, 59(3), 185-190. https://doi.org/10.4067/S0718-40262007000300004
Kamitani T, Matuso Y et al. (2014). Differentiation Between Benign Phyllodes Tumors and Fibroadenomas of the Breast on MR imaging, European Journal of Radiology, 83(8), 1344-1349. https://doi.org/10.1016/j.ejrad.2014.04.031
Karihtala P, Rissanen T et al. (2016). Male Malignant Phyllodes Breast Radiotherapy and Bicalutamide Treatment : Case report, Anticancer Research, 36(7), 3433-3436. https://ar.iiarjournals.org/content/36/7/3433.short
Nomura M, Inoue Y et al. (2006). A Case of Noninvasive Ductal Carcinoma Arising in Malignt Phyllodes Tumor, Racial and ethnic disparities in cancer, 13 (1), 89 – 94. https://doi.org/10.2325/jbcs.13.89
Parfitt J.R, Armstrong C et al. (2004). In-situ and Invasive Carcinoma within a Phyllodes Tumor Associated with lymph Node Metastases, World Journal of Surgical Oncology, https://wjso.biomedcentral.com/articles/10.1186/1477-7819-2-46
Pornchai S, Chirappapha P et al. (2019). Predictive Factors of Recurrence Following Surgical Treatment of Phyllodes Tumors in Ramathibodi Hospital, Practical Radiation Oncology, 44(1), 79-142. https://doi.org/10.1016/S0960-9776(19)30418-7
Santos, J.A. et al. (2007). Tumor Filodes de Mama : Características clínicas, en imagen y Anatomopatologicas a propósito de 18 casos, Chilean Journal of Radiology, 13(2), 90 -97. https://www.scielo.cl/scielo.php?script=sci_arttext&pid=S0717-93082007000200008
Spitaleri G, Toesca A et al. (2013). Breast Phyllodes Tumor : A review of literature and a Single Center Retrospective Series Analysis, Critical Reviews in Oncology/Hematology, 88(2), 427-436. https://doi.org/10.1016/j.critrevonc.2013.06.005
Sun L, zhu R et al. (2019). Coexisting DCIS and Phyllodes Breast Tumors in Young Chinese Women : Case Series, International Journal of Surgery Case Reports, 56, 13-16. https://doi.org/10.1016/j.ijscr.2019.01.045
Tan H, Zhang S et al. (2012). Imaging Findings in Phyllodes Tumors of the Breast, Discover This internationally Known Journal, 81(1), 62-69. https://doi.org/10.1016/j.ejrad.2011.01.085
Testori et al. (2015). Huge malignant Phyllodes Breast tumor : A Real Entity in a New era of Early Breast Cancer, World Journal of Surgical Oncology, 13, 81-82. https://doi.org/10.1186/s12957-015-0508-7
Wang Y, Zhang Y et al. (2018). Huge Bordeline Phyllodes Breast Tumor with Repeated Recurrences and Progression Toward More Malignant Phenotype : A case report and literature review, OncoTargets and Therapy,11, 7787-7793. https://doi.org/10.2147/OTT.S171714
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© Granthaalayah 2014-2022. All Rights Reserved.