Improvement Of The Life Quality For Laryngopharyngeal Reflux Patients After Receiving Proton Pump Inhibitor (PPI) Therapy At The Ent-Kl Polyclinic Of Uki Hospital January 2021 - February 2021
Abstract
Laryngopharyngeal reflux (LPR) is a condition in which gastric content reflux to the oesophagus and reaches larynx and pharynx so that mucous membranes of the larynx, pharynx, and other respiratory organs are inflamed. The symptoms of LPR can affect daily activities, resulting in a decrease in the quality of life (QOL) of the patients. Proton Pump Inhibitor (PPI) is the main therapy for patients with LPR. PPI can improve the symptoms experienced by patients with LPR. The objective of this research is to determine the QOL of patients with LPR after receiving PPI. This research's method is quasi-experimental studies using pre and post-test design from January 2021 to February 2021, in 18 patients were assessed for QOL scores using RSI. Each patient was administered lansoprazole 30 mg twice daily before meals for 14 days. Two times of observations are done, before therapy and 14 days after therapy. Data analysis using paired sample T-test. The result is that there is a significant improvement in QOL of patients with LPR on RSI scores after 14 days of administration of lansoprazole 30 mg. (p<0,05). It is concluded that PPI significantly improved the QOL of patients with LPR.
Keywords
Quality of Life (QOL), Laryngopharyngeal Reflux (LPR), Reflux Symptom Index, Proton Pump Inhibitor (PPI)
INTRODUCTION
Laryngopharyngeal reflux (LPR) is a condition in which stomach contents return to the oesophagus resulting in an inflammatory reaction the mucous membranes of the pharynx, larynx, and other respiratory organs. Gastric contents that return to the oesophagus and other respiratory organs cause coughing, hoarseness, a lump in the throat, difficulty swallowing, and sore throat (Zildzic, Masic, Salihefendic, Jasic, & Hajdarevic, 2020). The prevalence of LPR sufferers in the world ranges from 5-30% (Mishra, Agrawal, Chauhan, & Kaushik, 2020).
Laryngopharyngeal reflux is often undiagnosed due to the many symptoms and signs of this disease that overlap with other diseases such as upper respiratory tract infections, rhinitis, asthma, smoking, allergies, and excessive voice use (Fraser-Kirk, 2017). LPR diagnosis can be made using the Reflux Symptom Index (RSI), Reflux Finding Score (RFS), and the Dual-Sensor pH Probe (Kuo, 2019). The research conducted by Mallikarjunappa et al. proved that RSI has a sensitivity of 79.1% and a specificity of 83.7% in diagnosing LPR (Mallikarjunappa & Deshpande, 2020).
Management performed on LPR patients is diet modification, lifestyle changes, weight loss, exercise, medical therapy, and surgery. There are four classes of drugs that can be given as medical therapy to LPR patients, namely Proton Pump Inhibitor (PPI) class drugs, H2 receptor antagonists, prokinetic agents, and mucosal cytoprotectants. The main medical therapy for reflux disease is PPIs (Sirin & Öz, 2019).
LPR sufferers usually complain of hoarseness, globus sensation, coughing, dysphagia, sore throat, etc. The symptoms of LPR sufferers have many similarities to those of other diseases, so it is important to recognize LPR symptoms so that they do not cause a decrease in quality of life. The decline in quality of life in LPR patients is more often associated with the patient's symptoms than with the larynx's pathological findings (Febriyanti, 2014). LPR patients usually feel more than one symptom to interfere with patients in carrying out their daily activities. Additionally, a study found that one-third of LPR patients suffered from anxiety and experienced a significant reduction in social activity than those who did not experience LPR (Joo, Song, & Pae, 2017). The quality of life for LPR patients is usually lower than that of the general population.
Based on Lee et al research on changes in the quality of life of LPR patients after being given PPI therapy, there is a significant change in the RSI score of LPR patients after being given therapy (Gong et al., 2017). Another study regarding the improvement of the quality of life of LPR patients at RSUP H. Adam Malik Medan in 2014 proved that there was a significant change in the RSI score and the assessment in the following weeks (Lee, Lee, Kim, Kwon, & Eun, 2014). So far, no one has studied the improvement of the quality of life of LPR patients after being given PPI therapy at the UKI Hospital.
Based on the background description above, researchers are interested in improving patients' quality of life with laryngopharyngeal reflux after receiving Proton Pump Inhibitor (PPI) therapy ENT-KL polyclinic of RSU UKI for the period January 2021 - February 2021. The problem that will be answered in this research is "How is the quality of life of patients with laryngopharyngeal reflux after receiving Proton Pump Inhibitor (PPI) therapy at the ENT-KL polyclinic of UKI Hospital for the period January 2021 - February 2021? The purpose of this research is to "Knowing the quality of life of patients with laryngopharyngeal reflux after receiving Proton Pump Inhibitor (PPI) therapy at the ENT-KL polyclinic of RSU UKI for the period January 2021 - February 2021".
LITERATURE REVIEW
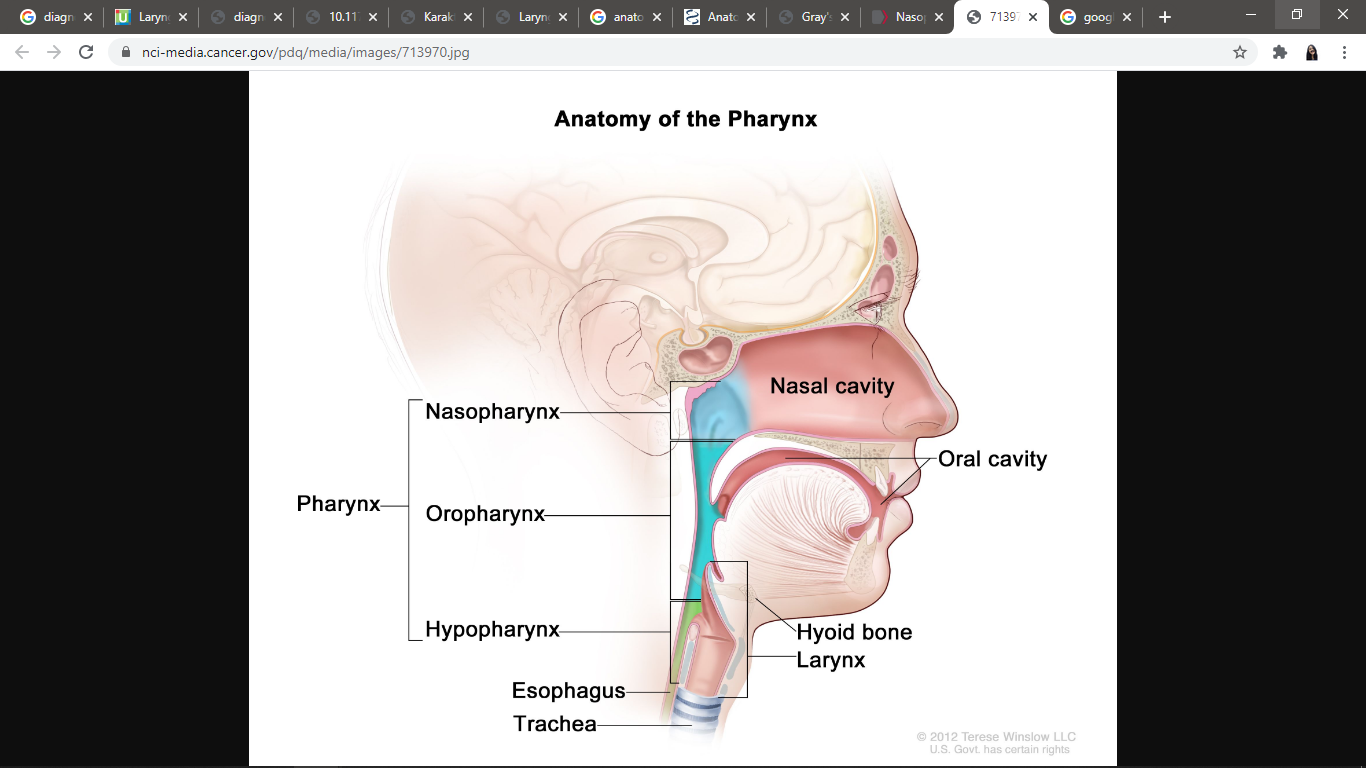
The pharynx is a funnel-shaped musculofascial tube, where the upper part is more comprehensive and lies just below the surface of the skull, and the lower part is narrower at the sixth cervical level vertebrae. The pharynx connects the oral cavity and nasal cavity with the larynx and oesophagus. The pharynx is divided into three parts, as shown in Figure 1, namely the nasopharynx (located just behind the aperture nasalis posterior or choanae), the oropharynx (located behind the oral cavity), and the laryngopharynx/hypopharynx (starting from aditus laryngis) (Albahout & Lopez, 2020; Drake, Drake, Vogl, & Mitchell, 2012).
The larynx is shaped like a musculoligamentous tube with cartilage that protects the inferior respiratory system. The larynx is an instrument that produces sound. There is moving up and forward from the larynx, so aryngic aditus closes, and the oesophagus opens when swallowing. The sensory and motor innervation of the larynx is innervated by the vagus nerve (N X) (Drake et al., 2012).
The oesophagus is a muscular tube that is between the pharynx and the stomach (Drake, Vogl, & Mitchell, 2015). The oesophagus starts from the Upper Esophageal Sphincter (UES) and ends at the Lower Esophageal Sphincter (LES). The function of the oesophagus is to carry food from the pharynx to the stomach. When food reaches the oropharynx, sensory stimulation occurs, which sends a signal to the swallowing centre in the brain stem, then the brain stem sends a message so that there is relaxation in the smooth muscle of the UES, which allows the bolus to pass through the UES and into the oesophagus. When the oesophagus performs its function, the UES prevents regurgitating food into the respiratory tract and prevents air from entering the digestive tract. A bolus that has entered the oesophagus triggers oesophagal peristalsis, where there is relaxation under the oesophagal area where the bolus is located, and there is a contraction above the area where the bolus is present so that the bolus can be pushed up into the lower oesophagus. When the bolus arrives at the end of the oesophagus, it will pass through the LES and enter the stomach. A smooth muscle helps keep the LES closed, thereby keeping the oesophagus from acid and other stomach contents components (Bajwa, Toro, & Kasi, 2020).
Laryngopharyngeal reflux (LPR) is a condition when there is a backflow of stomach contents into the larynx and pharynx, which causes tissue damage in the upper airway due to the acidity of the stomach acid (Nanda, 2016). RLF is often called extraesophageal reflux, supraesophageal reflux, or silent reflux (Kuo, 2019). There is a relationship between LPR and Gastroesophageal Reflux Disease (GERD), where 60% of GERD patients show LPR symptoms. However, LPR and GERD are different things.
In GERD patients, gastric acid reflux occurs only in the LES, while reflux that occurs in LPR patients reaches the UES and hypopharynx (Sa'an & N, 2017). In some cases, stomach contents can reach the nasal cavity and the eustachian tube through the ear, which can exacerbate rhinitis, sinusitis, or otitis media (Kuo, 2019).
Cherry first introduced the term LPR in 1968 as a larynx disease associated with reflux or reflux-related laryngeal disease. The current most widely used use of the term LPR was adopted from the American Academy in 2002 (Sirin et al., 2019). There was an increase of 500% in patients attending the otolaryngology department from 1990 to 2001 due to LPR (Priston, Thoen, Medeiros, Assunção, & Campagnolo, 2013). The prevalence of LPR varies by country. In Greece, it is 18.8%, in Latvia, it is 15%, in China it is 23.9%, and in the UK, it is 34.4% (Massawe et al., 2021). About 10% of patients who come to the otolaryngology department, more than 50% experience hoarseness associated with reflux disease (Somashekara & Kamath, 2015).
Several physiological barriers prevent LPR occurrence, namely LES, oesophagal clearance, saliva, gravity, and UES. When these barriers fail to carry out their physiological functions, there will be a backflow of gastric contents resulting in contact between the stomach contents and the laryngopharyngeal tissue, which causes damage to the epithelium, ciliary epithelial dysfunction, inflammation, and changes in sensitivity (Priston et al., 2013). The laryngeal mucosa is more sensitive to acids than the oesophagus. Oesophagal damage occurs when exposed to acid more than 50 times a day, while exposure to acid three times a week to the larynx can already cause damage to the larynx (Sirin et al., 2019).
Two mechanisms can irritate the laryngeal mucosa in LPR patients, namely the direct effect of exposure to gastric contents (gastric acid, pepsin, trypsin, bile salts, and some gastroduodenal proteins) on the laryngeal mucosa causing mucosal damage, inflammatory reactions, mucus dryness, thickening of the epithelium, and microtrauma. Another mechanism is the indirect effect of reflux of gastric contents, which stimulates the chemoreceptor mucosa in the oesophagus's distal part, triggering a vagal reflex and laryngeal mucosal secretions, coughing, globus sensation, and throat clearing (Lechien et al., 2019; Lechien, Saussez, Harmegnies, Finck, & Burns, 2017). This direct or indirect mechanism can cause irritation, leading to oedema of the vocal cords, pseudosulkus of the vocal cords, contact ulcers, granulomas associated with other LPR symptoms hoarseness, globus pharyngeus, and sore throat (Kuo, 2019).
The most common symptoms in people with LPR are persistent cough, globus sensation, sore throat, throat clearing (clearing the throat), difficulty swallowing, heartburn, and hoarseness. Globus sensation is the sensation of a lump or foreign object in the throat (Somashekara et al., 2015). Heartburn occurs in 75% of GERD patients, whereas only about 40% of LPR patients report heartburn (Kuo, 2019). It is essential to differentiate the clinical manifestations of GERD and LPR. The main difference between GERD and LPR is the dysfunctioning oesophagal sphincter muscle, wherein GERD there is LES dysfunction, and in LPR, the dysfunction is UES. Reflux episodes in LPR patients are usually intense and occur during the day when symptoms usually worsen when standing. LPR patients usually deny symptoms of esophagitis or heartburn, whereas most GERD patients complain about it (Fraser-Kirk, 2017; Kuo, 2019).
In diagnosing LPR, a careful history is needed based on the clinical symptoms felt by the patient. Belafsky et al. developed a validated questionnaire, namely RSI, as in Table 1 . This questionnaire contains nine questions regarding the symptoms felt by the patient. The patient will be asked to give 0 to 5 points for each question on the questionnaire, and then all the points are added up to see the patient's total points. If the patient's final RSI score is> 13, then the patient is diagnosed with LPR (Satish, Datta, Manjula, Poojari, & Molluru, 2016).
|
Reflux Symptom Index (RSI) |
|||||||
|
Do you suffer one of the following within this month? |
Skor |
||||||
|
1 |
Hoarseness/voice problems |
0 |
1 |
2 |
3 |
4 |
5 |
|
2 |
Often clears throat / expels throat mucus |
0 |
1 |
2 |
3 |
4 |
5 |
|
3 |
Excess mucus / Post Nasal Drip (PND) |
0 |
1 |
2 |
3 |
4 |
5 |
|
4 |
Swallowing Difficulty |
0 |
1 |
2 |
3 |
4 |
5 |
|
5 |
Cough after eating/lying down |
0 |
1 |
2 |
3 |
4 |
5 |
|
6 |
Difficulty breathing / chocking |
0 |
1 |
2 |
3 |
4 |
5 |
|
7 |
Annoying cough |
0 |
1 |
2 |
3 |
4 |
5 |
|
8 |
A lump in the throat |
0 |
1 |
2 |
3 |
4 |
5 |
|
9 |
Heartburn, chest pain, indigestion, acid regurgitation |
0 |
1 |
2 |
3 |
4 |
5 |
Information
-
no complaints
-
mild, complaints can be ignored 1x in 1 month
-
moderate, complaints can not be ignored, 1x in 1 week
-
severe complaints affect lifestyle, several times a week
-
very heavy, complaints significantly affect the lifestyle, every day
-
severe complaints and persist all day long
Physical examination of LPR patients is carried out using the aid of a device, namely a laryngoscope, to view the throat and larynx. The findings of laryngoscopy used to diagnose LPR are non-specific signs of laryngeal irritation and inflammation (Priston et al., 2013). Apart from the RSI, there is an instrument developed by Belafsky, namely the RFS. This instrument is used to measure the severity of laryngeal inflammation as seen by laryngoscopic examination. There are 8 points assessed in the RFS as in table 2, namely subglottic oedema, ventricular obliteration, erythema or laryngeal hyperemia, vocal cord oedema, diffuse laryngeal oedema, posterior commissural hypertrophy, granuloma or granulation tissue in the larynx, and thick endolaryngeal mucus. Patients will be diagnosed with LPR if the total RFS score obtained is> 7 (Kuo, 2019).
|
Symptoms |
Score |
|
|
1 |
Subglotic edema / vocal pseudosulcus |
0 = nothing |
|
|
|
2 = exist |
|
2 |
Ventricular obliteration |
0 = nothing |
|
|
|
2 = partial |
|
4 = complete |
||
|
3 |
Erythema / hyperemia |
0 = nothing |
|
|
|
2 = arytenoid only |
|
4 = diffuse |
||
|
4 |
Vocal cord oedema |
0 = nothing |
|
|
|
1 = light |
|
2 = moderate |
||
|
3 = weight |
||
|
4 = polypoid |
||
|
5 |
Diffuse laryngeal edema |
0 = nothing |
|
|
|
1 = light |
|
2 = moderate |
||
|
3 = weight |
||
|
4 = obstruction |
||
|
6 |
Posterior commissural hypertrophy |
0 = nothing |
|
|
|
1 = light |
|
2 = moderate |
||
|
3 = weight |
||
|
4 = obstruction |
||
|
7 |
Granuloma / granulation |
0 = nothing |
|
|
|
2 = exist |
|
8 |
Endolaryngeal thick mucus |
0 = nothing |
|
|
|
2 = exist |
The most common conditions are erythema/hyperemia, vocal cord oedema, and diffuse laryngeal oedema on physical examination (Mallikarjunappa et al., 2020).
The supporting examination that can be done to confirm LPR diagnosis is a dual-sensor pH probe which is also the gold standard in diagnosing LPR (Kuo, 2019). This examination is carried out by checking the pH for 24 hours through two electrodes inserted intranasally and placed 5 cm above the LES and 0.5-2 cm above the UES. Although this examination is the standard gold examination in establishing an LPR diagnosis, it is not a definitive test and has caused controversy (Sa'an et al., 2017).
Another test that can be done to make a diagnosis of LPR is the PPI test. The PPI test is an empirical therapy used as an alternative diagnostic modality to confirm LPR diagnosis in a non-invasive and straightforward manner. This test is done by giving the PPI at a twice-daily dose for two to three months. However, the literature states that giving omeprazole 40 mg per day for 14 days has the same sensitivity and specificity as a 24-hour metric pH test (Febriyanti, 2014; Priston et al., 2013).
Management for LPR patients includes lifestyle changes in dietary modification, exercise, and weight loss. Besides, there are also medical therapy and surgery. Evaluation of Quality of life is critical in assessing the success of therapy. Quality of life concerns health issues and describes a person's ability to lead a productive life in the economic and social fields (Febriyanti, 2014). The World Health Organization (WHO) defines the quality of life as each individual's perception of their position in the context of the cultural and value systems they live in and concerning their goals, hopes, standards and concerns (Lechien et al., 2019).
More than 50% of LPR patients complain of chronic cough and voice problems. It causes the patient inconvenience in carrying out daily life. Therefore, LPR patient care should improve the patient's symptoms to improve the patient's quality of life. Some of the instruments used to measure the quality of life of LPR patients are RSI, Laryngopharyngeal Reflux-Health Related Quality of Life (LPR-HRQL), and Short Form 12 (SF-12) (, 1997).
RESEARCH METHOD
This research is a quasi-experimental study with a pre and post-test design. This study used data taken directly from the ENT-KL polyclinic of UKI Hospital using the RSI questionnaire to measure patients' quality of life with laryngopharyngeal reflux. The location of data collection for this research was carried out in the ENT-KL polyclinic of RSU UKI. Data collection and implementation of this study were carried out from January 2021 - February 2021. This study population were all laryngopharyngeal reflux patients who came to the ENT-KL polyclinic of UKI Hospital in January 2021 - February 2021. Sampling in this study used the accidental sampling technique so that the sample size taken for this study was determined based on the study's time. Any number of laryngopharyngeal reflux patients who come to the ENT-KL clinic of UKI Hospital during January 2021 - February 2021 can be sampled in this study. The research instrument used was the Reflux Symptom Index (RSI) questionnaire. Data processing that has been collected through medical records is carried out using the IBM SPSS (Statistical for Social Science) program for Windows edition 23.0 and the Microsoft Office Excel 2019 program.
RESULT AND DISCUSSION
This study was obtained using primary data obtained through filling out the RSI questionnaire by taking anamnesis on laryngopharyngeal reflux patients who came to the ENT-KL polyclinic of RSU UKI in January 2021 - February 2021. Observations of Quality of life were carried out using an RSI questionnaire assessed before and after therapy for two weeks. In this study, there were 18 research subjects.
|
Characteristics |
Frequency (patients) |
Percentage (%) |
|
Gender |
|
|
|
Male |
7 |
38,69 |
|
Female |
11 |
61,1 |
|
Age |
|
|
|
20 year |
3 |
16,7 |
|
21 year |
11 |
61,1 |
|
22 year |
2 |
11,1 |
|
23 year |
2 |
11,1 |
|
Total |
18 |
100 |
Table 3 hows the study subjects' characteristics, where out of a total of 18 study subjects, 11 patients (61.1%) were female, and seven patients (38.69%) were male. When viewed from their age, the highest age distribution in this study was 21 years, namely 11 patients (61.1%), with an average age of 21.17 years.
|
Main complaint |
Frequency (patients) |
Percentage (%) |
|
Hoarseness |
2 |
11,1 |
|
Clears throat a lot |
2 |
11,1 |
|
Post-Nasal Drip (PND) |
2 |
11,1 |
|
Annoying Cough |
3 |
16,7 |
|
A feeling of a lump in the throat |
4 |
22,2 |
|
Heartburn |
5 |
27,8 |
|
Total |
18 |
100 |
Table 4 hows that this study's main complaint was heartburn, which was five patients (27.8%), followed by a lump in the throat in 4 patients (22.2%), and a cough that bothered three patients (16.7%). Other main complaints were hoarseness found in 2 patients (11.1%), frequent clearing in 2 patients (11.1%), and PND was found in 2 patients (11.1%).
|
|
Mean |
Frequency (Patients) |
Std. Deviation |
|
Pre-Therapy Score |
16,78 |
18 |
2,102 |
|
Post-Therapy Score |
9,94 |
18 |
2,155 |
Through Table 5 , it is known that there is a decrease in the mean value of the RSI score in research subjects before and after giving PPI therapy for 14 days.
|
|
Mean |
Std. Deviation |
t |
df |
p-value |
|
Pre and Post Therapy Score |
6,833 |
1,383 |
20,968 |
17 |
0.000 |
Based on the statistical analysis results in Table 6 regarding the improvement of the quality of life of patients with laryngopharyngeal reflux after receiving PPI therapy, there is a significant change in patients' quality of life after PPI therapy with a p-value <0.05.
This study found that the research subjects were more female than male, namely 11 female patients (61.1%) and seven male patients (38.69%). It is consistent with Somashekara & Kamath's research in 2015, which showed that LPR incidence was more common in women (56.66%) than men (43.33%) (Somashekara et al., 2015). Other studies also show that LPR is dominated by women, namely 85.7%, while men are only 14.3% (Silva, Duprat, Machado, Melo, & Ribeiro, 2021). Another research conducted at RSUP DR. M. Djamil Padang for the period 2017 showed that LPR patients were found in 66.27% women and only 33.73% in men with a ratio of male to female ratio of 1: 2 (Sa'an et al., 2017).
The higher incidence of LPR in women than men is because women have a higher stress level than men. Stress will stimulate the vagus nerve through sympathetic innervation in the hypothalamus to produce acetylcholine. Acetylcholine will then stimulate histamine to stimulate gastric parietal cells increasing gastric acid production (Febriyanti, 2014). Besides, hormonal factors in women also play an essential role in increasing gastric acid secretion. Hormonal pathways mediated by the hypothalamus, anterior pituitary gland, and Adrenocorticotropic Hormone (ACTH) can stimulate the adrenal glands to secrete cortisol adrenals, which can stimulate parietal cells and peptic glands to produce HCl and pepsin (Pramana, Muyassaroh, & Antono, 2015). It could be the reason why LPR is more experienced by women than men.
This study's age characteristics were mostly found at the age of 21 years (61.1%). This study's results are following the results of research conducted on populations in India where the incidence of LPR was mostly found in the 21-30 year age group, namely 42% (Mishra et al., 2020). The age of 21 years is classified as productive age. Individuals at productive age are often faced with challenges, pressures, and tasks that can be a source of stress for the individual if the individual cannot handle them. Excessive stress and duties on an individual can affect his diet (Tussakinah, Masrul, & Burhan, 2017). Research shows that lifestyle changes, one of which is diet, can improve LPR symptoms. It means that diet can affect the incidence of LPR. A diet that can cause LPR symptoms is eating at least two hours before bedtime, consuming too much coffee, alcohol and carbonated drinks, and reducing spicy foods (Kuo, 2019). While we are eating, there will be an increase in stomach acid. Gastric distension occurs when the food we eat reaches the stomach, and this causes stimulation of the vagus nerve to release acetylcholine. Furthermore, acetylcholine will stimulate histamine release, which will stimulate gastric parietal cells to secrete gastric acid (Wilson & Stevenson, 2019). Besides, consumption of coffee, alcohol, and carbonated drinks can cause a decrease in the tone of the oesophagal sphincter, which can trigger reflux of stomach contents (Newberry & Lynch, 2019).
This study's main complaint was heartburn (27.8%), followed by a lump in the throat (22.2%). It is following research conducted by Mallikarjunappa and Deshpande, who got 93.9% of heartburn symptoms (Mallikarjunappa et al., 2020). Another study conducted by Mishra et al. also showed that heartburn was the most common symptom experienced by LPR patients, as many as 95 patients (38%) (Mishra et al., 2020).
LPR patients who complain of heartburn may be associated with any abnormalities that may also occur in the oesophagus (Febriyanti, 2014). LPR is often considered a manifestation of extraesophageal reflux, so LPR patients may also experience heartburn and acid regurgitation symptoms (Stinnett, Dhillon, & Akst, 2018). Heartburn or heartburn occurs due to repeated exposure to stomach acid in the oesophagus due to reflux. It causes an inflammatory reaction in the oesophagus and causes heartburn (Clarrett & Hachem, 2018).
The mean RSI score before therapy in this study was 16.78 with a standard deviation of 2.102. After 14 days of therapy with lansoprazole twice a day before meals, there was a decrease in the mean RSI score to 9.94 with a standard deviation of 2.155. It is according to the research conducted by Febriyanti, where there was a significant difference in mean, namely 18.47 with a standard deviation of 4.35 at the start of the assessment and 10.94 with a standard deviation of 3.90 after two weeks of therapy with omeprazole 20 mg twice. the day before meals (p <0.05) (Febriyanti, 2014). Another study conducted by Lee et al. Also stated a significant change in the RSI score after receiving PPI therapy for four weeks, from 13.15 with a standard deviation of 8.68 to 10.03 with a standard deviation of 8.97 (p. <0.01) (Lee et al., 2014). It is also in line with a study conducted by Silva et al., which showed a significant decrease in the RSI score after PPI administration, from the mean initial score before treatment of 16.0 to 10.5 after being given therapy (p <0.001) (Silva et al., 2021).
Clinical manifestations of LPR may emerge from direct exposure to gastric acid to the upper aeoridigestive tract mucous and may also be caused by vagal reflexes emerged from chemoreceptors in the distal esophagus stimulated by gastric acid reflux. Both of these can cause damage to the mucous membrane leads to inflammatory reaction and causing symptoms experienced by LPR patients (Mishra, Agrawal, & Artham, 2020). In addition, the inflammatory reaction that occurs in allergic patients is related to the incidence of LPR. There is a study that found that 85% of LPR patients have allergic rhinitis (RA) (Alharethy et al., 2018). The upper and lower respiratory tracts are unified, where the larynx is a structure that connects the upper and lower respiratory systems. If there is an inflammatory reaction in one part of the respiratory tract, it can also cause inflammation in other parts (Campagnolo & Benninger, 2019).
Patients who have atopic conditions mostly experience chronic respiratory diseases such as asthma and RA. In RA patients, there is an increase in the frequency of swallowing due to an itching sensation in the throat and PND. The increasing frequency of swallowing can exacerbate reflux by increasing the frequency of transient lower-esophageal sphincter relaxations (TLESRs). Inflammation of the nasal mucosa that occurs in RA patients can also have the same effect on the laryngeal mucosa, such as mucosal edema, excessive mucus secretion, and congestion that can cause LPR symptoms. Eosinophils are a major component that plays a role in inflammatory reactions and also found in the esophageal mucosa of GERD patients. The release of histamine from mast cells can increase the onset of GERD patients through LES contractions (Kung et al., 2019).
The clinical manifestations of LPR are non-specific symptoms. Even so, these symptoms can affect the quality of life of the sufferer. Globus pharyngeus or globus sensation and hoarseness are the most frequent clinical manifestations in LPR patients (Fraser-Kirk, 2017). Other clinical manifestations that can also appear in LPR patients are throat clearing, dysphagia, and chronic cough (Somashekara et al., 2015). Besides, heartburn is also found in LPR patients, although this symptom is more common in GERD patients. The symptoms experienced by LPR patients can interfere with patients in carrying out their daily activities.
Due to the non-specific symptoms of LPR, it is often late in diagnosis and causes delays in its management. It affects the patient's quality of life, where the patient's ability to work is impaired and can increase financial losses (Massawe et al., 2021). The quality of life for LPR patients is usually lower than that of the general population. It harms the quality of life of the sufferer. LPR can also be a predisposing factor for various types of laryngeal diseases such as reflux laryngitis, subglottic stenosis, laryngeal carcinoma, granuloma, contact ulcers, and vocal nodules (Putri, Yusmawan, & Yunika, 2018). Therefore, the diagnosis of LPR must be made as soon as possible.
RSI and RFS are the instruments most widely used to diagnose LPR. Several supporting tests can be done to help establish the diagnosis of LPR, such as dual sensor pH probes, empirical therapy with PPIs, multichannel intraluminal impedance-pH monitoring (MII-pH Monitoring), Oropharyngeal pH Monitoring, detection. Pepsin and bile salts, and a histopathological examination can also be performed. However, a study concluded that RSI is a simple tool to diagnose and evaluate therapy in LPR patients without the need for invasive procedures. RSI is easier to use to evaluate therapy because the improvements that arise can be assessed more quickly than using findings at the time of physical examination (Zildzic, Masic, Salihefendic, Jasic, & Hajdarevic, 2020).
The primary therapy that is usually given to LPR patients is PPI. Ideally, LPR patients take PPIs twice daily to ensure the effectiveness of the drug. This drug inhibits H +, K +, and ATPase in the stomach cell walls, thereby reducing gastric acid secretion, reducing pepsin activity, and blocking the inflammatory response to reduce the occurrence of direct tissue damage (Lechien et al., 2018). PPI class drugs are effective for at least 8-12 weeks. Omeprazole and lansoprazole are the types of PPI that are used earlier, where pharmacokinetically, lansoprazole is considered superior because it has high bioavailability, can interact less with other drugs, and does not reduce the absorption of B12.
The study conducted by Putri et al. showed that LPR patients treated using lansoprazole and omeprazole both showed a significant decrease in RSI scores, so it was concluded that there was no significant difference in the effectiveness of omeprazole and lansoprazole in reducing the RSI score of LPR patients. Besides, this study also found a significant improvement in the symptoms found in RSI in the LPR patient group treated with lansoprazole (p <0.005), while there was no significant improvement in some of the symptoms found in RSI, such as symptoms of coughing, PND. Furthermore, bothersome cough in patients being treated with omeprazole (p> 0.005). Another study using pantoprazole also showed a significant improvement in RSI scores after receiving therapy (p <0.001). There was also a significant (p <0.001) improvement in RSI symptoms after three months of therapy in the study (Lechien et al., 2018). Despite using different types of PPIs for LPR therapy, all types of PPIs have the same efficacy for acid-induced treatment. In this study, there was a significant decrease in the RSI score, which illustrated the improvement of the study subjects' complaints after receiving PPI therapy, so it can be concluded that PPI therapy can improve the quality of life of LPR patients.
CONCLUSION
Based on the results of this study, it can be concluded that: a) The characteristics of LPR patients in the ENT-KL polyclinic of UKI Hospital in January 2021 - February 2021, most of them were female and 21 years old; b) The main complaint among LPR patients who came to the ENT-KL clinic at UKI Hospital in January 2021 - February 2021 was heartburn; c) There was a decrease in the mean RSI score before and after therapy in LPR patients who came to the ENT-KL polyclinic of UKI Hospital in January 2021 - February 2021; and d) There was a significant improvement in the quality of life of LPR patients who came to the ENT-KL clinic at UKI Hospital in January 2021 - February 2021 after receiving PPI therapy (p = 0.000).

