|
|
|
|
ANALYSIS OF OPTIC CHIASM RADIATION DOSE FOR NASOPHARYNGEAL CANCER (NPC) PATIENTS WITH INTENSITY MODULATED RADIOTHERAPY (IMRT) TECHNIQUE BASED ON DOSE VOLUME HISTOGRAM (DVH) GRAPH FOR THERAPY USING LINAC
Azibatul Habibah 1
![]()
![]() ,
Evi Setiawati 1
,
Evi Setiawati 1![]()
![]() , Asep Yoyo Wardaya 1
, Asep Yoyo Wardaya 1![]()
![]() ,
Agus Margiantono 2
,
Agus Margiantono 2![]()
![]() ,
Galih Puspa Saraswati 3
,
Galih Puspa Saraswati 3![]()
![]()
1 Department of Physics Diponegoro University, Semarang , Indonesia
2 Department of Electrical Engineering ,
Semarang University , Indonesia
3 Radiology of Ken Saras Hospital.
Semarang , Indonesia
|
|
ABSTRACT |
||
|
Motivation/Background: Radiotherapy is the standard therapy that uses ionizing rays for the treatment of malignancies. However, in some cases of nasopharyngeal cancer (NPC), the location of the tumor pushes to the base of the brain until it reaches the optic chiasma. The optic chiasm as part of a healthy organ around the target irradiation becomes a dangerous organ or a risk organ (OAR) so it needs to be considered in the case of radiation therapy for NPC. This study aims to consider dosing in patients to fulfill radiation protection. IMRT technique is believed to maximize the success of therapy in cases of NPC. Results: The results of the analysis showed that of the 15 patient data analyzed, there were 10 patients with a percentage of 66.67% who received radiation doses that were in accordance with the ICRU Report 62 reference (95-107%) while patients who received less than optimal doses (< 95%) there were 5 people with a percentage of 33.33% while the maximum dose received by OAR for the optic chiasm in NPC patients who had complied with QUANTEC rules overall there were 7 patients with a percentage of 46.67% while there were 8 patients who received doses exceeding the QUANTEC limit with a percentage of 53 ,33% risk of receiving radiation side effects by 7-20%.. Conclusions: there were patients who received doses exceeding QUANTEC as much as 53.33% |
|||
|
Received 03 November 2022 Accepted 04 December 2022 Published 17 December 2022 Corresponding Author Evi Setiawati, evi_setiawati_msi@yahoo.com
DOI 10.29121/ijetmr.v9.i12.2022.1265
Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2022 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
Keywords: Radiotherapy ,
DVH, NPC, OAR , PTV |
|||
1. INTRODUCTION
Cancer is
the leading cause of death after heart disease and stroke. There are several
types of cancer with various cases that can attack children, women, and men.
Cancer cases that usually attack women are breast cancer with the first most
cancer cases in Indonesia. Meanwhile, cancer cases that usually attack men are
nasopharyngeal cancer because apart from the Epstein-Barr virus, most of the
triggers are environmental factors such as cigarette smoke Kementrian Kesehatan (2020).
nasopharyngeal
carcinoma (NPC) is one of the most common types of malignant tumor cases in the
world, especially in Southeast Asia which has the highest incidence, with
Indonesia being the second country after Malaysia with the highest incidence of
NPC Sinambela and Supriana
(2018). In Indonesia, based on hospital-based
cancer registration report data for the period of January 2020, there were 20,503 cancer cases out of a total of 20,503 cases, there were 1,276 cases of
nasopharyngeal cancer which was the most common case suffered by male patients,
namely 889, followed by colorectal cancer as many as 820 patients Sardjito (2020). Corroborated by GLOBOCAN data (Global
Burden Cancer) in 2014 recorded 87,000 new cases of nasopharyngeal cancer every
year that 61,000 occur in men and 26,000 in women with 51,000 cases of death
from nasopharyngeal cancer with 36,000 in men and 15,000 in women Kemenkes (2017). From these data it can be concluded that
the ratio of nasopharyngeal cancer patients between women and men is 1:2.
Nasopharyngeal
cancer is one of the most confusing cancers in terms of early detection. The
presence of the tumor is difficult to identify clearly because the anatomical
factor of the nasopharynx is hidden behind the palate and is located under the
skull base and is connected to many important organs in the skull Pratiwi and Imanto
(2020). Important organs around the nasopharynx
area, which in this case are risk organs, commonly referred to as Organs At
Risk (OAR), are very likely to be exposed to radiation, so it is necessary to
pay attention to the large dose that will be received by the organ so that it
does not exceed the rules as regulated in the ICRU Report 62 of 1999. Based on
this, the most likely modality in cancer treatment is radiotherapy.
Radiotherapy is
a standard therapy that uses ionizing rays for the treatment of malignancy so
that it becomes the right choice for cases of NPC with its anatomical location
which is relatively radiosensitive and difficult to perform surgery or
chemotherapy. Anatomical factors and patterns of spread of nasopharyngeal
cancer cells and postoperative risks make surgery difficult. Another reason for
using radiotherapy is because with chemotherapy the cancer cells do not
disappear completely because only microscopic tumors are eradicated so that
chemotherapy is not optimal enough and is still controversial Kodrat and Novirianthy
(2016). The radiation technique used is external
radiation or external beam therapy with light sourced from Linear Accelerator (LINAC).
LINAC is an
accelerator that can accelerate electrons to have a kinetic energy of up to 25
MeV Panular (2012). The use of LINAC can be in the form of
electron or photon radiation with a certain energy according to therapeutic
needs. Radiation treatment planning techniques for linac-based irradiation that
can be applied to NPC cases are usually 3DCRT (3 Dimensional Conformal
Radiation Therapy) and IMRT (Intensity Modulated Radiotherapy). In some cases
of nasopharyngeal cancer, the location of the tumor pushes to the base of the
brain until it reaches the optic chiasm. The optic chiasm is a very important
part of the brain when it comes to processing visual information from the
retina, the optic chiasm is the meeting point between the left and right optic
nerves Foroozan et al. (2016). In this case, the optic chiasm as part
of a healthy organ around the radiation target becomes an organ at risk (OAR)
so it needs consideration in the case of radiation therapy for nasopharyngeal
cancer. If the optic chiasma is exposed to excessive radiation, it will cause
problems for the patient in the form of symptoms of decreased visual acuity and
can even cause blindness. For this case of NPC, it is more advisable to use the
IMRT technique.
IMRT is
believed to be able to maximize the success of therapy with computerized
methods in terms of the formation of a high-accuracy irradiation field
according to the shape of the tumor that is read from the results of the
CT-simulator examination and the provision of non-uniform radiation intensity
according to the needs of each target part in each direction of the irradiation
field Febrietri et al. (2020). This is able to optimize the radiation
dose that will be received by the Planning Target Volume (PTV) and minimize the
radiation received by healthy tissue/OAR so that a Dose Volume Histogram (DVH)
graph is obtained with satisfactory results.
Dose Volume
Histogram (DVH) is a graph obtained from the results of the irradiation
planning or Treatment Planning System (TPS) which displays the radiation dose
distribution at each radiation irradiation target, namely PTV and OAR [10]. In
the process of making TPS using the 3DCRT and IMRT techniques, there are 3
principles that need to be considered for radiation protection, namely
limitation, optimization, and justification. The optimization principle must be
met so that the dose of PTV as the cancer target to be irradiated gets maximum
radiation so that it is optimal in killing the cancer cells, therefore the dose
of PTV radiation is regulated in ICRU Report 62 of 1999, namely (95-107)% which
means PTV received a minimum dose of 95% and a maximum dose of 107%. Meanwhile,
the principle of limitation must be met so that the dose of OAR can be
minimized so that healthy organs are endeavored to receive the minimum dose
possible. Based on this, the reference regarding the tolerance dose of OAR
refers to the rules in the Quantitative Analysis of Normal Tissue Effects in
the Clinic (QUANTEC). QUANTEC states that the radiation dose that can be
received by the optic chiasma of nasopharyngeal cancer patients is Dmax <55
Gy, which means the maximum radiation dose that can be received by the optic
chiasm is less than 55Gy or 5,500 cGy with a toxicity rate of <3% while for
a toxicity rate of 3-7%. , the radiation dose that can be received by the optic
chiasma of nasopharyngeal cancer patients is dmax 55-60 Gy, which means the
maximum radiation dose that can be received by the optic chiasma is 55Gy to 60
Gy.
In this study, an analysis of radiation protection achievements was carried out in nasopharyngeal cancer patients, especially at Ken Saras Hospital, Ungaran, Kab. Semarang by analyzing the radiation dose received by the target cancer cells (PTV) and the optical chiasma as OAR which was observed by looking at the DVH graph of the TPS results with the Intensity Modulated Radiotherapy (IMRT) technique. This research is expected to be one of the considerations for evaluation for Ken Saras Hospital, Ungaran, Semarang in giving radiation doses so that they can apply the principle of radiation protection which is useful for optimizing the health of post-therapy nasopharyngeal cancer patients.
2. MATERIALS AND METHODS
This research at the Radiology Installation of the Radiotherapy Unit II Ken Saras Hospital, Semarang, Central Java. In this study, secondary data was used by looking at the DVH (Dose Volume Histogram) graph from the results of radiation planning for NPC patients using the IMRT (Intensity Modulated Radiotherapy) technique. Data analysis was carried out on PTV and OAR dose values NPC patients at Ken Saras Hospital on the DVH chart that was adjusted to the wishes used, namely The International Commission on Radiation Units and Measurements (ICRU) Report 62 (1999) for PTV doses and QUANTEC for doses OAR.
3. RESULTS AND DISCUSSIONS
Dose Volume
Histogram (DVH) has been successfully obtained from the manufacture of
radiation planning or the Treatment Planning System (TPS) in patients according
to their respective nasopharyngeal cancer cases using the Intensity Modulated
Radiation Therapy (IMRT) technique. The obtained DVH shows the coordinates for
the cancer target (PTV) and healthy organs around the cancer (OAR).
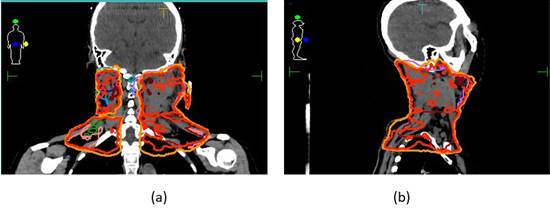
Figure 1
|
Figure
1 Anatomical Location of Nasopharyngeal Cancer Patient #1 (a) Coronal
(b) Sagittal |
For example,
patient #1 data shown in Figure 1 is a DVH image from patient #1 TPS which shows the anatomy of
nasopharyngeal cancer shown by red, yellow, green, pink, light blue, and purple
lines. It can be seen that the irradiation area carried out in the neck area
does not reach the head area, meaning that the organs in the head area remain
safe from radiation exposure by only receiving relatively small doses.
Figure 2

|
Figure
2 Anatomical Location from Patient's #1 of Nasopharyngeal Cancer in
Direction Axial |
From Figure 2, it can be seen that there is a part of the head which is a healthy organ around the irradiation target that receives scattered radiation as well as the optical chiasm which is indicated by a light blue line. It can be interpreted that the optic chiasma in patient #1 received a radiation dose whose magnitude can be seen in the following DVH graph.
Figure
3

|
Figure
3 Graph of Dose Volume Histogram (DVH) Patient #1 |
Based on the
DVH graph in Figure 3, it can be seen that the color lines that
indicate the PTV dose are optimal enough as shown by a perfectly distributed
curve showing a uniformly high dose throughout the volume, which is in the form
of a step function and a steep slope indicates that most of the volume is have
the same dose. Likewise, the optical chiasm is indicated by the blue curve on
the left. For healthy organs around cancer or commonly known as Organ at risk
(OAR), DVH must have a concave appearance. This shows that the radiation dose
received by OAR is relatively small Walter and Miller (2019).
Figure 4

|
Figure
4 Radiation Dose Distribution from Patient #1 |
Figure 4 shows the radiation dose distribution of
patient 1 who underwent radiotherapy irradiation with the IMRT technique. The
table shows the distribution of radiation on several organs that are the target
of irradiation or commonly referred to as PTV. In the case of nasopharyngeal
cancer patients, PTV is not only in one organ but depends on the spread of the
patient's cancer. Based on these data, PTV has received doses above 95%, namely
99.86%, 98.69%, 92.01%, 98.30%, 99.40%, and 97.00%. It means that the PTV value
in the patient indicates that the patient received the maximum radiation dose
and complies with the provisions of ICRU report 62 of 1999. Therefore, the
treatment of this patient can be said to have fulfilled the optimization
principle in terms of radiation protection. However, it is also seen that the
patient received a scattering of radiation dose of 7,000 cGy this will also affect the dose received by
the surrounding healthy organs including the optic chiasm.
Table 1
|
Table 1 PTV Radiation Dose for Nasopharyngeal Cancer Patients |
||
|
PTV Dose |
Frequency |
Percentage |
|
Suboptimal (< 95%) |
5 |
33.33 % |
|
Optimal (95 % - 107 %) |
10 |
66.67 % |
|
total |
15 |
100 % |
Table 1 shows that of the 15 patient data that
was carried out in the study, the PTV value in patients indicating that the
patient received the maximum radiation dose (95% - 107%) and fulfilled the provisions
of the ICRU Report 62 of 1999 there were 10 people with a percentage of 66.67%
while patients who received less than the maximum radiation dose (< 95%)
there were 5 people with a percentage of 33.33%.
Table 2
|
Table 2 Radiation Dose Data for Nasopharyngeal Cancer
Patients |
|||
|
|
OAR Dose |
Frequency |
Percentage |
|
Valid |
according to QUANTEC rules |
7 |
46.67 |
|
Miss-ing |
Exceeding the QUANTEC rule |
8 |
53.33 |
|
|
Total |
15 |
100 |
Table 2 shows that the maximum dose received by
OAR for the optic chiasm in nasopharyngeal cancer patients at Ken Saras
Hospital, Ungaran, Semarang, where the study was conducted, there were 7
patients who received doses according to QUANTEC rules with Dmax
<6,000 cGy and from the
data obtained there were 8 patients who received doses exceeding the QUANTEC
limit with Dmax> 6,000cGy.
The dose received
by the optic chiasm is highly dependent on the location of the tumor as PTV,
the closer it is to the optic chiasma, the more at risk of receiving an
excessive dose. In addition, in order to keep maximizing the PTV dose, the PTV
dose is increased so that the radiation dose received by OAR is higher but
remains within rational limits in the sense that it is still at the tolerated
dose. However, there is still the possibility of OAR getting radiation side
effects.
In detail, the
radiation dose received by nasopharyngeal cancer patients who were researched
at Ken Saras Hospital, Ungaran, Semarang are as follows:
Table 3
|
Table 3 Radiation Dose Data for Nasopharyngeal Cancer
Patients |
||||
|
Patient |
PTV Dose (%) |
ICRU 62 year 1999 |
Dmax
OAR (cGy) |
QUANTEC year 2013 |
|
Patient #1 |
92.01 |
× |
533 |
√ |
|
Patient #2 |
93.02 |
× |
1,19.5 |
√ |
|
Patient #3 |
96.12 |
√ |
7,017.2 |
× |
|
Patient #4 |
99.99 |
√ |
6,476.6 |
× |
|
Patient #5 |
98.28 |
√ |
6,151.9 |
× |
|
Patient #6 |
91,81 |
× |
5,983.1 |
√ |
|
Patient #7 |
98 |
√ |
4,965.3 |
√ |
|
Patient #8 |
95.07 |
√ |
6,603.1 |
× |
|
Patient #9 |
89.83 |
× |
2,637.5 |
√ |
|
Patient #10 |
97.89 |
√ |
5,581.9 |
√ |
|
Patient #11 |
96.51 |
√ |
6,164.4 |
× |
|
Patient #12 |
96.64 |
√ |
6,087.1 |
× |
|
Patient #13 |
95.93 |
√ |
7,656.1 |
× |
|
Patient #14 |
98.74 |
√ |
6,233.9 |
× |
|
Patient #15 |
93.78 |
× |
2,457.4 |
√ |
In this study,
8 of 15 patients with optic chiasm received doses exceeding the Dmax limit set
by QUANTEC (Quantitative Analysis of Normal Tissue Effects in the Clinic) as
seen from the data in Table 3 above. According to a QUANTEC review, an
entire optic chiasm organ dose of <5,000 cGy was associated with a <1% risk of blindness. In fact, blindness
is quite rare up to a dose of 5,000 cGy. Between 5,500-6,000 cGy the risk of blindness is around
3-7%. At doses >6,000 cGy,
the risk of damage is greatly increased by 7-20%. This shows that when the
optical chiasma receives radiation with a certain dose, it will still have a
stochastic effect, namely radiation side effects that can only be minimized,
not eliminated. From the analysis of the data obtained, it turns out that there
are 8 cases of patients who are at risk of experiencing side effects of
radiation with a toxicity rate of >7% due to receiving doses of radiation
exposure exceeding 6,000 cGy.
Taking into
account the radiation dose received by the optic chiasm as a healthy organ
around the cancer target that needs to be protected will greatly affect the
achievement of radiation protection so that the possibility of stochastic
effects can be minimized.
The side effect
of radiation that may be experienced by patients is radiation necrosis with the
main symptom in the form of decreased visual acuity and can even cause
blindness. Blindness or loss of vision occurs due to radiation-induced optic
neuropathy, but not all patients whose optic chiasm receives excessive doses
experience this. According to Zaccagna et al. (2018) radiation necrosis does not only occur
due to radiation therapy, but also occurs in patients who have undergone
surgery for sellar, parasellar, or skull base tumors.
Table 4
|
Table 4 Radiation Dose from Optic chiasm as OAR of Nasopharyngeal Cancer
Patients |
|||||
|
Patient |
Dmax (cGy) |
QUANTEC rule |
Risk
of Blindness |
||
|
Dmax |
Dmax 5,500-6,000cGy |
Dmax>6,000
cGy |
|||
|
Patient #1 |
533 |
√ |
1% |
||
|
Patient #2 |
1,195 |
√ |
1% |
||
|
Patient #3 |
7,017.2 |
√ |
>7% |
||
|
Patient #4 |
6,476.6 |
√ |
>7% |
||
|
Patient #5 |
6,151.9 |
√ |
>7% |
||
|
Patient #6 |
5,983.1 |
√ |
3-7% |
||
|
Patient #7 |
4,965.3 |
√ |
1% |
||
|
Patient #8 |
6,603.1 |
√ |
1% |
||
|
Patient #9 |
2,637.,5 |
√ |
1% |
||
|
Patient #10 |
5,581.9 |
√ |
3-7% |
||
|
Patient #11 |
6,164.4 |
√ |
>7% |
||
|
Patient #12 |
6.087.1 |
√ |
>7% |
||
|
Patient #13 |
7,656.1 |
√ |
>7% |
||
|
Patient #14 |
6,233.9 |
√ |
>7% |
||
|
Patient#15 |
2,457.4 |
√ |
1% |
||
One of the
factors causing the radiation dose value received by cancer patients is the
level of cancer stage classification of each patient. Nasopharyngeal cancer
patient at Ken Saras Hospital, Ungaran, Kab. Semarang has received a dose of
66-70 Gy with a dose of 1.75-2Gy/fraction, which means that all analyzed
patients have a high-risk level of cancer in the subclinical area. According to
the radiotherapy principles in the Guidelines for the Management of
Nasopharyngeal Cancer by the National Cancer Management Committee, the
definitive curative radiation dose for PTV at high risk is from 66 Gy to 70 Gy
(1.8-2Gy/fraction) depending on the comfort level of the patient's positioning.
daily. Tumors involve on the one hand that the optic chiasm becomes a critical
normal tissue structure at risk in which patients can be threatened with
blindness as a result of therapy by receiving high enough doses of the optic
chiasm, some patients exceed the QUANTEC limit due to tumors in high risk
regions, so that informed consent is necessary and for the sake of To protect
the contralateral optic structure, it is necessary to limit the dose to the
optic chiasm. However, with a limit of 1 mm is considered sufficient to protect
the critical normal tissue structure (AOR) in the area around the brain stem
and spinal cord Kemenkes, and Kanker
(2017).
4. CONCLUSIONS AND RECOMMENDATIONS
Based on the
results obtained in the study, several conclusions can be formulated are the
results of radiation dose analysis conducted on 15 nasopharyngeal cancer
patients at Ken Saras Hospital, Ungaran, Semarang showed that there were 5 patients
who received a less than optimal dose based on ICRU Report 62 of 1999 which was
<95% while for OAR chiasma optics there were 8 patients who received
radiation doses exceeding the QUANTEC limit, which was >6,000 cGy, which means that 8 patients had a
level of cell damage toxicity. of >7%, which is about 7-20% the possibility
of experiencing a stochastic effect in the form of Radiation Necrosis.
CONFLICT OF INTERESTS
None.
ACKNOWLEDGMENTS
The authors would like to thank those who have helped the author in the process of research, analysis and script writing, including Diponegoro University, Ken Saras Hospital in Ungaran, Semarang central of java who have assisted the author in obtaining the necessary data, to my supervisor for comments that greatly improved the manuscript.
REFERENCES
Febrietri, O., Milvita, D., and Diyona, F. (2020).
Analisis Dosis Radiasi Paru-Paru Pasien Kanker Payudara Dengan Teknik
Three-Dimensional Conformal Radiation Therapy (3D-CRT) Berdasarkan Grafik Dose
Volume Histogram (DVH). Jurnal Fisika Unand, 9(1), 110–117. https://doi.org/10.25077/jfu.9.1.110-117.2020.
Foroozan, R., Bhatti, M. T., Falardeau, J., Gordon, L. K., Lee, M. S., Subramanian, P. S., and Kawasaki, A. (2016). Neuro-Opthalmology. In L. B, Cantor, C. J. Rapuano, and G. A. Cioffi, Basic And Clinical Science Center. American Academy Of Ophthalmology, 29–34.
Kemenkes, R. I. (2017). Kanker Nasofaring. Jakarta : Komite Penanggulangan Kanker Nasional (KPKN).
Kemenkes, R. I., and Kanker, K. P. (2017). Nasional (KPKN). Kanker Nasofaring
Kementrian Kesehatan, R. I. (2020). Jenis Kanker Ini Rentan Menyerang Manusia.
Kodrat, H., and Novirianthy, R. (2016). Prinsip Dasar Radiotherapi. Jurnal Medika, 318–323.
Panular, B. D. (2012). Perbandingan Hasil Pengukuran Parameter Berkas Sinar-X dan Elektron Keluaran Pesawat LINAC Menggunakan Detektor Matriks dan Fantom Air [Tesis], Program Studi Magister Fisika, Kekhususan Fisika Medis, FMIPA. Universitas Indonesia.
Pratiwi, A., and Imanto, M. (2020). Karsinoma Nasofaring Dengan Multiple Cranial Nerve Palsy Pada Pasien Wanita Usia 52 Tahun. Medula, 609–615.
Sardjito, (2020). FKKMK UGM. Laporan Kanker Berbasis Rumah Sakit (RKBR) Dr.Sardjito.
Sinambela, A., and Supriana, N. (2018). Revolusi Teknik Radioterapi Pada Karsinoma Nasofaring. Radioterapi and Onkologi Indonesia, 9(1), 20–28. https://doi.org/10.32532/jori.v9i1.71.
Walter, and Miller. (2019). Textbook of Radiotherapy Radiation Physics, Therapy and Oncology, 8nd ed. Elsevie.
Zaccagna, F., Pizzuti, V., Barone, D. G., Siotto, P., Saba, L., Raz, E., Matys, T., and Massoud, T. F. (2018). In and around the optic chiasm:a pictorial review of neuroimaging. Neurographics, 1–2. https://doi.org/10.3174/ng.1700068.
|
|
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© IJETMR 2014-2022. All Rights Reserved.


