ShodhKosh: Journal of Visual and Performing ArtsISSN (Online): 2582-7472
|
|
PREDICTIVE MODELLING FOR STRESS MANAGEMENT OF HEALTHCARE EMPLOYEES
J. Katyayani 1![]()
![]() ,
Dr. Ch. Varalakshmi 2
,
Dr. Ch. Varalakshmi 2![]()
1 Department
of Business Administration, Sri Padmavati Mahila Viswavidyalayam,
Tirupati, Andhra Pradesh, India
2 Assistant
Professor, Department of MBA, Andhra Loyola College, Andhra Pradesh, India
|
|
ABSTRACT |
||
|
The healthcare
sector and healthcare professionals were essential during the COVID-19
epidemic. There is an enormous need for workers in the healthcare sector due
to the necessity of industry. Professionals in this field must endure a great
deal of pressure at work due to irregular hours and demanding schedules. The
goal of this study is to evaluate the stress levels and stress management
strategies of healthcare workers. This study focuses on a
number of factors, including the age, gender, and marital status of
the employees as well as physical working conditions, timely deadlines,
co-worker cooperation, individual health issues, working conditions, improved
compensation and training for job performance, and cooperation within the
family. How they are employing methods that reduce stress to manage their
stress. |
|||
|
Corresponding Author J.
Katyayani, DOI 10.29121/shodhkosh.v5.i1.2024.1694 Funding: This research
received no specific grant from any funding agency in the public, commercial,
or not-for-profit sectors. Copyright: © 2024 The
Author(s). This work is licensed under a Creative Commons
Attribution 4.0 International License. With the
license CC-BY, authors retain the copyright, allowing anyone to download,
reuse, re-print, modify, distribute, and/or copy their contribution. The work
must be properly attributed to its author.
|
|||
|
Keywords: Covid19, Healthcare, Stress Management |
|||
1. INTRODUCTION
The healthcare industry, sometimes referred to as the medical industry or the health economy, is the collection and integration of economic sectors that offer products and services for the treatment of patients in the areas of palliative, preventative, rehabilitative, and curative care. A vast array of industries that offer products and services to treat patients are included in the healthcare sector. This covers activities including patient treatment, disease prevention, and the provision of palliative and rehabilitative medicine. Globally, the healthcare industry has increased significantly, with a projected value of $12 trillion by 2022, up from $8.5 trillion in 2018. The overall healthcare market in India is expected to reach $372 billion by 2022, growing at a compound annual growth rate (CAGR) of 22%. Globally, the healthcare industry has grown significantly, with a projected value of $12 trillion by 2022, up from $8.5 trillion in 2018. The total healthcare market in India is projected to reach $372 billion by 2022, growing at a compound annual growth rate (CAGR) of 22%. Globally, the healthcare industry has grown significantly, with a projected value of $12 trillion by 2022, up from $8.5 trillion in 2018. India's healthcare industry is now one of the biggest in terms of jobs and income. Hospitals, medical equipment, clinical trials, outsourcing, telemedicine, medical travel, health insurance, and medical devices are all included in the category of healthcare. The robust coverage, services, and rising spending by both public and private entities are driving the rapid growth of the Indian healthcare sector.
The public and private sectors make up the two main parts of India's healthcare delivery system. The government's public healthcare system, or Primary Healthcare Centres (PHCs) in rural regions, provides basic healthcare facilities. It consists of a small number of secondary and tertiary care facilities in major cities. The bulk of secondary, tertiary, and quaternary care facilities are run by the private sector, with tier-I and tier-II cities and metro areas bearing the brunt of this concentration.
India has a plethora of highly qualified medical experts, which gives it a competitive advantage. When compared to its Asian and Western counterparts, India is likewise reasonably priced. Surgery in India is roughly ten times less expensive than in the US or Western Europe. Due to the inexpensive cost of healthcare, the nation has seen an increase in medical tourism, drawing in people from all over the world. Moreover, because clinical research in India is relatively inexpensive, the country has become a center for foreign players' R&D efforts. Stress is a pervasive issue in the healthcare sector, affecting the well-being of healthcare professionals and, consequently, patient care outcomes. This literature review synthesizes key findings from studies and research articles that explore stress management strategies, causes of stress, and the impact of stress on healthcare professionals within various contexts.
1) Causes of Stress in Healthcare Professionals: Healthcare professionals face numerous stressors that can impact their physical, emotional, and psychological health. Studies consistently identify factors such as heavy workloads, long hours, patient care responsibilities, interpersonal conflicts, and lack of support as significant contributors to stress (Siddiqui et al., 2020; Shanafelt et al., 2017). These stressors can lead to burnout, compassion fatigue, and decreased job satisfaction among healthcare workers.
2) Impact of Stress on Healthcare Professionals: The impact of stress on healthcare professionals is profound and multifaceted. Research indicates that chronic stress can lead to physical health problems such as hypertension, cardiovascular disease, and musculoskeletal disorders (Firth-Cozens, 2019). Moreover, stress is associated with increased absenteeism, turnover rates, and decreased quality of patient care (McManus et al., 2021). Addressing stress among healthcare professionals is crucial not only for their well-being but also for maintaining high standards of patient care and organizational performance.
3) Stress Management Strategies: Effective stress management strategies are essential for mitigating the negative effects of stress on healthcare professionals. Research highlights several approaches that can help reduce stress and promote resilience. These include organizational interventions such as improving work environments, implementing supportive leadership, and fostering a culture of well-being (Panagioti et al., 2017). Individual-level strategies such as mindfulness-based interventions, stress management training, and self-care practices are also effective in enhancing coping mechanisms and reducing stress levels (West et al., 2018).
4) Organizational Interventions and Policies: Organizations play a critical role in addressing stress among healthcare professionals through policy development and implementation. Studies underscore the importance of organizational support systems, including employee assistance programs, peer support networks, and mental health resources (Salyers et al., 2020). Creating a positive work culture that prioritizes work-life balance, job autonomy, and recognition can significantly contribute to reducing stress and improving overall job satisfaction among healthcare professionals.
5) Future Directions and Recommendations: Despite the growing body of research on stress management in the healthcare sector, several challenges and opportunities for future research and practice remain. Longitudinal studies are needed to assess the long-term effectiveness of stress management interventions. Moreover, addressing systemic issues such as healthcare system reforms, workload management, and professional development opportunities is crucial for sustainable stress reduction strategies (Dyrbye et al., 2017
2. STRESS MANAGEMENT
The tools, approaches, or methods that lessen stress and lessen the detrimental effects that stress has on your physical or mental health are referred to as stress management techniques. There are numerous methods for handling stress. These consist of behavioural, emotional, and mental techniques.
3. REVIEW OF THE LITERATURE
Amutha’s (2022) study states that an employee's stress level varies based on their industry and type of job. Particularly in the healthcare sector, factors including positive self-evaluation, resignation, and seeking for social assistance can have an impact on an employee's physical, mental, and social well-being. As a result, the work environment has a significant impact on employees' mental and emotional health. Coping mechanisms for stressful situations play a critical role in the interaction between individuals and their environment. They thus have a significant effect on both physical and mental wellbeing. The development and expansion of programs for psychological assistance and counselling in the healthcare industry.
According to a study by Lesley and Tolu published in 2023, up to 70% of healthcare professionals report high levels of stress and burnout, which negatively impacts patient care. Research sometimes concentrates on stresses in a specific environment or in relation to the pandemic, which restricts our comprehension of a more complete picture of the stressors faced by healthcare professionals. There are three primary categories of stresses: those related to work (49%), those related to personal life (32%), and stressors involving the intersection of work and personal life (19%). New insights into daily pressures that aren't easily categorized into one sector of life but instead could be connected to job, personal life, or the intersection of both have come from this study.
According to Ruotsalainen's (2015) study, a lack of skills, organizational issues, and a lack of social support at work can all contribute to occupational stress in healthcare personnel. Distress, burnout, psychosomatic issues, and a decline in living quality and service delivery could result from this. Based on Stefan's study from 2022, there appears to be no substantial relationship between the level of demands and occupational health, but a larger degree of control is linked to better health. The results of the correlation study showed that there is a mixed relationship between the quality management values and demand, although there is a correlation with control.
According to White's estimate from 2021, stress costs US$191 billion a year and has an impact on healthcare workers (HCWs) in the United States. Burnout affects between 30% and 50% of healthcare professionals. According to an evaluation of a rural hospital system in the United States, 94% of employees suffered from unfavourable health outcomes.
The study conducted by Nwobodo in 2023 observed that Stress management techniques to deal with issues like limited medical equipment, unfavourable work environments, low pay, and heavy workloads for Nigerian healthcare personnel. It advocates for a thorough overhaul of the healthcare system in order to raise the standard of care and better the health of medical personnel. The tactics include developing support networks, encouraging work-life balance, offering counselling and mindfulness training, and setting up support and resilience programs. Reforming the health system should place a high priority on allocating significant funds for sufficient medical resources and equipment, enhancing workplace conditions, addressing pay inequality, and enforcing workload guidelines. Nigeria may develop a more robust and healthy healthcare workforce by putting these initiatives into practice, which would ultimately improve healthcare services.
Research of Burman (2018) indicates that the effects of work-related stress extend beyond an employee's physical and mental health to include their job performance and productivity. Employees who experience work-related stress are more likely to suffer from several health conditions, including blood pressure, depression, anxiety, and nervousness.
The study conducted by Sanghmithra in 2021 observed that shown that stress which can be managed in a healthy manner can actually lead to increased brain functioning, a stronger immune system and better preparation for stress in the future, which can positively affect emotional health with your work and home life. But if stress level goes out of control, it can cause medical problems such as depression, anxiety, fluctuating BP and more. This is when interventions to improve the organization of work and reduce the impact of stressful jobs on our health can be conducted in a wide variety of ways. Alterations can be made at the level of the job through laws and regulations.
Stress management is a critical concern in the healthcare industry due to its pervasive impact on healthcare professionals' well-being and patient outcomes. This review synthesizes recent literature to explore effective strategies and interventions aimed at mitigating stress among healthcare workers.
1) Causes
and Impact of Stress
· Healthcare professionals face numerous stressors including high workload, long hours, patient care demands, administrative burdens, and emotional challenges (Kumar, 2018; Shanafelt et al., 2017). Chronic stress can lead to burnout, reduced job satisfaction, increased medical errors, and compromised patient safety (West et al., 2016; Dyrbye et al., 2018).
2) Interventions
for Stress Management
·
Organizational Interventions:
· Workload Management: Implementing workload caps, optimizing scheduling, and utilizing team-based care models have shown promise in reducing stress (Rathert et al., 2018).
· Supportive Work Environment: Cultivating a supportive culture, promoting teamwork, and providing resources for mental health support can buffer against stress (Panagioti et al., 2017).
·
Individual Interventions:
· Mindfulness and Resilience Training: Programs that incorporate mindfulness techniques and resilience-building skills have demonstrated effectiveness in enhancing coping mechanisms and reducing stress levels (Burton et al., 2017; Verweij et al., 2018).
· Stress Reduction Techniques: Techniques such as relaxation exercises, cognitive-behavioral therapy (CBT), and stress management workshops have been found beneficial (Krasner et al., 2009; West et al., 2016).
3) Technological
Innovations
· Advancements in technology have introduced digital platforms and applications aimed at supporting stress management in healthcare professionals. These include mobile apps for meditation, stress tracking tools, and virtual support communities (Blake et al., 2020).
4) Barriers
and Challenges
· Despite the growing recognition of stress in healthcare settings, barriers such as inadequate resources, time constraints, and resistance to change hinder the widespread adoption of stress management interventions (Bleich et al., 2018).
5) Future
Directions
· Future research should focus on longitudinal studies to assess the long-term efficacy of stress management interventions. Additionally, exploring the role of leadership support and policy changes in fostering a culture of well-being is crucial (Panagioti et al., 2017).
4. HYPOTHESIS OF THE STUDY
There is a significant relationship between employees age, gender, marital status, physical working conditions, timely deadlines, co-worker cooperation, individual health issues, working conditions, improved compensation and training for job performance, and cooperation within the family on employee’s workplace stress management
5. OBJECTIVES OF THE STUDY
To analyse the impact of employees age, gender, marital status, physical working conditions, timely deadlines, co-worker cooperation, individual health issues, working conditions, improved compensation and training for job performance, and cooperation within the family on employee’s workplace stress management
6. RESEARCH DESIGN
The descriptive research is used for this study. The study considering various employees of healthcare industry. 260 healthcare sector employees from NTR District participated in this survey. Snowball sampling technique is used for this study. A structured questionnaire distributed to all the respondents
7. DATA ANALYSIS
Table 1
|
Table 1 Impact
of Employee’s Gender on Their Stress Management at Workplace |
||||
|
Factor |
Mean |
Standard deviation |
F-Value |
Significance |
|
Gender |
3.37 |
0.929 |
308 |
0.579 |
Table-1 represents employee Gender is insignificant with their Stress Management at Workplace
Table 2
|
Table 2 Impact of
Employee’s Age on Their Stress Management at Workplace |
||||
|
Factor |
Mean |
Standard deviation |
F-Value |
Significance |
|
Age |
3.37 |
0.929 |
44.33 |
0.001 |
Table-2 represents employee Age is significant with their Stress Management at Workplace
Table 3
|
Table 3 Impact
of Employee’s Marital Status on Their Stress Management at Workplace |
||||
|
Factor |
Mean |
Standard deviation |
F-Value |
Significance |
|
Marital status |
3.37 |
0.929 |
67.678 |
0.001 |
Table-3 represents employee Marital Status is significant with their Stress Management at Workplace
Table 4
|
Table 4 Impact
of Employee’s Physical Working Environment on their Stress Management at
Workplace |
||||
|
Standard deviation |
F-Value |
Significance |
||
|
Physical Working Environment |
3.37 |
0.929 |
37.5 |
0.001 |
Table-4 represents employee Physical Working Environment is significant with their Stress Management at Workplace
Table 5
|
Table 5 Impact of Employee’s Timely Deadlines on Their Stress Management at Workplace |
||||
|
Factor |
Mean |
Standard deviation |
F-Value |
Significance |
|
Timely Deadlines |
3.37 |
0.929 |
38.5 |
0.001 |
Table-5 represents employee Timely Deadlines is significant with their Stress Management at Workplace
Table 6
|
Table 6 Impact
of Employee’s Co-Worker’s Cooperation on Their Stress Management at Workplace |
||||
|
Factor |
Mean |
Standard deviation |
F-Value |
Significance |
|
Co-Worker’s Cooperation |
3.37 |
0.929 |
101.625 |
0.001 |
Table-6 represents employee Co-Worker’s Cooperation is significant with their Stress Management at Workplace
Table 7
|
Table 7 Impact
of Employee’s Health Issues on Their Stress Management At
Workplace |
||||
|
Factor |
Mean |
Standard deviation |
F-Value |
Significance |
|
Employee’s Health Issues |
3.37 |
0.929 |
43.656 |
0.001 |
Table-7 represents employee Health is significant with their Stress Management at Workplace
Table 8
|
Table 8 Impact of Employee’s Working Conditions on Their Stress Management at
Workplace |
||||
|
Factor |
Mean |
Standard deviation |
F-Value |
Significance |
|
Working Conditions |
3.37 |
0.929 |
45.357 |
0.001 |
Table-8 represents employee Working Conditions is significant with their Stress Management at Workplace
Table 9
|
Table 9 Impact of Employee’s Compensation on Their Stress Management at Workplace |
||||
|
Factor |
Mean |
Standard deviation |
F-Value |
Significance |
|
Employee’s Compensation |
3.37 |
0.929 |
23.323 |
0.001 |
Table-9 represents employee Compensation is significant with their Stress Management at Workplace
Table 10
|
Table 10 Impact
of Employee’s Training on Their Stress Management at Workplace |
||||
|
Factor |
Mean |
Standard deviation |
F-Value |
Significance |
|
Employee’s Training |
3.37 |
0.929 |
11.272 |
0.001 |
Table-10 represents employee training is significant with their Stress Management at Workplace
Table 11
|
Table 11 Impact
of Employee’s Family Cooperation on Their Stress Management at Workplace |
||||
|
Factor |
Mean |
Standard deviation |
F-Value |
Significance |
|
Employee’s Family
Cooperation |
3.37 |
0.929 |
66.146 |
0.001 |
Table-11 represents employee family cooperation is significant with their Stress Management at Workplace
8. RESEARCH FRAMEWORK
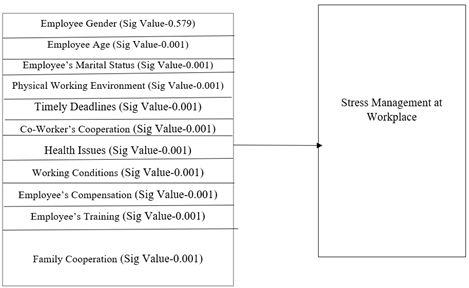
Figure 1
|
Figure 1 Research Framework for Stress Management |
From the above model employee age, gender, marital status of the employees as well as physical working conditions, timely deadlines, co-worker cooperation, individual health issues, working conditions, improved compensation and training for job performance, and cooperation within the family are predictive variables and employee Stress Management at Workplace is the outcome variable.
9. CONCLUSION
The survey included individuals from several categories, including nursing superintendents, technologists, district quality managers, dieticians, infection control nurses, executive administrators, dialysis technicians, quality executives, assistant managers, pharmacists, finance managers, and doctors. To implement better stress management techniques in the health care industry, the following practices must be implemented: meditation or yoga classes in health care settings because in health care, professionals do not focus on stress management. Making supporting staff and administrative staff meet frequently off the job and discuss things outside the box, on-the-job trainings, and live problem solving will reduce stress. Employing health care professionals in higher-level positions allows them to gain an improved awareness of the health sector outside the business perspective. In conclusion, stress management in the healthcare sector is a complex and pressing issue that requires concerted efforts from healthcare organizations, policymakers, and healthcare professionals themselves. By implementing evidence-based stress management strategies, fostering supportive work environments, and advocating for systemic changes, stakeholders can mitigate the impact of stress on healthcare professionals and enhance the quality of patient care.
CONFLICT OF INTERESTS
None.
ACKNOWLEDGMENTS
None.
REFERENCES
Kumar S. (2018).
Burnout and doctors: prevalence, prevention,
and intervention. Healthcare.
|
|
 This work is licensed under a: Creative Commons Attribution 4.0 International License
This work is licensed under a: Creative Commons Attribution 4.0 International License
© ShodhKosh 2024. All Rights Reserved.

